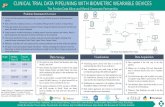
Academic Report On The Pitfalls Of Clinical Trial For Medical Devices
-
Upload
asia-medical-supplies -
Category
Documents
-
view
38 -
download
0
Transcript of Academic Report On The Pitfalls Of Clinical Trial For Medical Devices

Academic Report On The Pitfalls Of Clinical Trial For Medical Devices
1.0 BACKGROUND OF THE REPORT
The author has based on the case study known as the Blinded Evaluation of Laser Intervention Electively For Angina Pectoris (BELIEF) trial reported by Nordrehaug and Fauls (1999). Case name is known as A Randomized, Sham-Procedure-Controlled Trial of Percutaneous Myocardial Laser Therapy (PML)
1.1 BACKGROUND OF THE CLINICAL TRIAL
There are a majority of patients at a growing rate who have medically refractory angina caused by diffuse coronary artery disease who are not suitable for percutaneous coronary intervention (PCI) or coronary artery bypass graft surgery (CABG). Prior to the development of the surgical transmyocardial laser revascularization, treatment option are limited to this subset of patients.
Prior to the year 1995, the Norwegian Ministry of Health (NMOH) prohibited the use of the surgical transmyocardial laser revascularization (TMR) as a routine clinical option cited the concerns regarding the procedural morbidity and mortality.
Only in year 1999, an independent expert consensus panel of cardiothoracic surgeons, cardiologists, and physiologist commissioned by The Norwegian Ministry of Health (NMOH) went through an extensive review of the non-clinical and clinical literature to revisit the feasibility, suitability and acceptability of surgical transmyocardial laser revascularization (TMR) procedure that was banned since 1995.
The panel eventually concluded that transmyocardial laser revascularization (TMR) consistently provides significant symptomatic relief and lifted the ban on prohibiting surgical transmyocardial laser revascularization (TMR) as a routine clinical option for patients with severe angina.
However, the panel couldn’t figure out the mechanism for transmyocardial laser revascularization (TMR) on how it delivered its clinical benefits. This unknown mechanism together with the lack of evidence discounting the placebo effect as the primary mechanism for the observed clinical improvement still limited the routine clinical use of the technology.
1.2 OBJECTIVES OF BELIEF TRIAL
To address the panel’s finding and to workaround the unethical practice of a Sham transmyocardial laser revascularization (TMR) trial. Nordrehaug and Fauls (1999) designed the BELIEF clinical trial as a randomized, two-arms, double-blind clinical trial to control for patient bias (the placebo effect) and investigator bias (assessment bias) in determining the clinical benefit of Percutaneous Myocardial Laser (PML) treatment.
A sample size of minimum 82 patients that have to be randomized into comparable key baseline characteristics were established to detect a clinically relevant difference in the proportion of patients with at least a one class improvement in Canadian Cardiovascular Society grading (CCS) angina class. All assessment were conducted by blinded, independent assessors.
1.3 PARTICIPATING STAKEHOLDERS
All aspects of the BELIEF trial were conducted in Norway with the participation of Haukeland University Hospital and Ullevaal University Hospital. The trial were conducted under the governance of the Institutional Ethics Review Committees and according to the guideline set forth in the Declaration of Helsinki.
The Biostatistic Department of the University of Bergen assisted in generating of the randomization code for the procedural blinding and randomization process.
Funding for the BELIEF trial was provided through a grant from the Bergen Norway Heart Foundation.
EdwinNgChunPeng_RAPS_Module 2_Term Report_2015_2016 pg. 1

The CardioGenesis Corporation’s Axcis PML system was chosen for the BELIEF trial because of its proven clinical benefits in a randomized, controlled, open-label trial.
1.4 PROCEDURAL DETAILS
The Axcis PML system consists of the holmium:yttrium-aluminum-garnet laser, an electrocardiography (ECG) monitor, and the sterile delivery system. The laser is a portable, self-contained unit that has a maximum therapeutic output of 6W and consists of a laser console and a footswitch.
The limitation of the Axcis PML system is the continuous output of the laser energy that penetrates the tissue to a depth of around 5 to 6cm even though the physical penetration has stopped. As a result, clinical application is limited to eligible areas of the left ventricular wall that are at least 8mm thick to reduce the potential for pericardial perforation.
In the PML group, pulsed-laser energy was delivered to the endocardium through the laser catheter to create a nontransmural channel. For the Sham group, the procedure (invasive) was identical except that there was no laser energy delivered to the patient when the interventionalist activated the footswitch.
1.5 PROCEDURAL METHODS
A total of eighty-two qualified patients with severe angina (20 PML and 42 Sham) undergo the trial. The PML group were assigned to receive Myocardial Laser channels, pulsed laser energy was delivered to the endocardium through the laser catheter to create a nontransmural channel. For the Sham group, they were subjected to the blinded Sham procedure (known as placebo) that was identical except there was no laser energy delivered.
All patients were in Canadian Cardiovascular Society grading (CCS) Class III or IV at baseline, with distributions comparable between group.
The primary endpoint was the change in Canadian Cardiovascular Society grading (CCS) angina class from 3-months, 6-months, and a 1-year angina class assessment.
1.6 RESULTS
79 out of the 82 patients randomized were available for follow-up through 1 year.
There were no crossover of patients from the Sham group to the treated group, no withdrawals and none of the patients received additional revascularization procedures and change of medication during the study.
Results through 1 year of Mean angina class improvement at 3 months, angina class improved to 2.3 +- 1.0 in the PML group and to 2.7 +- 0.9 in the Sham group.
At 6 months, Angina class was reduced significantly more in the PML group at 2.0+- 1.1 as compared to the Sham group at 2.7+- 0.9. The PML group were observed to have improved by at least 1 class (63% vs. 36%) and by at least 2 classes (40% vs. 12%) from baseline.
At the 1 year assessment, the trend continued for the PML group, one or more class improvement (63% vs. 38%) over the Sham group and two or more class improvement (35% vs. 14%) over the Sham group.
The procedural success, in this case, study was defined as the completion of the entire procedure through patient discharge in the absent of death or perforation.
At 1 year, cardiac event-free survival as defined as the absence of death, MI, perforation, stroke/TIA and angina requiring rehospitalization was similar between groups. In the PML group, there were no death or MI, only a case of single perforation, a patient suffered a stroke at 3 months and was unable to travel for further follow-ups and three other patients were hospitalized for angina during follow-up.
EdwinNgChunPeng_RAPS_Module 2_Term Report_2015_2016 pg. 2

On the other hand, in the Sham group, 2 patients deaths occurred, one procedurally and the other at 3 months owing to a suspected MI. 1 patient was reported with MI, TIA, and atrial fibrillation. 3 other patients were hospitalized for angina during follow-up.
1.7 CONCLUSION FROM BELIEF TRIAL
Nordrehaug and Fauls (1999) concluded their unique design, well-focused and excellent follow-up randomized, double-blind, Sham-controlled BELIEF trial mitigated the influence of other potentially confounding factors such as changes in medical therapy or incomplete ascertainment.
As a result, the positive 1-year results are free from any concern of placebo effect as a primary mechanism.
Together with the superior Axcis PML system intended to achieve the stated primary endpoint. The clinical benefit is indeed attributed to the effect of treatment and beyond placebo.
2.0 DISCUSSION ON THE PITFALLS OF BELIEF TRIAL
The BELIEF trial is in the opinion of the author a first and foremost new trial and therapy in the year 1996 without any precedent case for reference and to improvise. However, Nordrehaug and Fauls were capable enough to design and implemented the trial while adhering to the regulation and expectation of the many different stakeholders and opinion leaders namely: the Norwegian Ministry of Health (NMOH), CardioGenesis Corporation, Bergen Norway Heart Foundation, The Ethics Review Committees of both Haukeland University Hospital and Ullevaal University Hospital.
For that reason, the author’s purpose of this paper is not to criticize but to raise more questions, suggest recommendation and to provide some corresponding answer from the finding in the various referencing source. The following statements on the pitfalls of the BELIEF trial are based on observation by the author based on others case-study and are not conclusively in nature.
2.1 UNINTENTIONALLY DISCLOSURE
In this BELIEF trial, to assure blinding of the patients, there was great effort to conceal the laser console and the laser operator by placing them behind an opaque curtain out of view in the cardiac catheterization laboratory. Furthermore, music was played during the procedure to mask over the audible feedback from the laser system that could reveal the randomized assignment.
The author believed that the laser inducing smell and even surgical smoke will be observed by the treating investigators, staffs and PML group participants, whereas for Sham group participants it is the lack of smell and smoke. Cooper et al. (2014) commented that trial participants can comments, share and feedback on the different characteristics of the intervention among treating investigators and others participants which may eventually reveal the group allocation.
The author believed that by maintaining a Confidential Disclosure Agreement (CDA) or Non-Disclosure Agreement (NDA) among all parties should be able to address the revelation pitfall and at least minimize the chances of occurring.
2.2 SHORT-TERM RELIEF?
Galiñanes, et al. (2004) reported PML treatment is an effective short-term therapy for the relief of angina and the improvement of the quality of life of patients with diffuse coronary artery disease who cannot receive angioplasty or bypass graft surgery. However, its efficacy is limited and most patients remain with some degree of angina. This clinical benefit is partly lost by 42 months follow-up suggesting that the improvement may be transient.
EdwinNgChunPeng_RAPS_Module 2_Term Report_2015_2016 pg. 3

Based on the finding above, the author finds that the Norwegian Ministry of Health (NMOH) expert consensus panel should have also included clinical questions such as how the duration, frequency and number of follow-up will affect and impact on the assessment of a longer-term clinical benefit for the BELIEF trial to address.
2.3 DIFFERENT STARTING LINE = DIFFERENT RESULT?
Based on the BELIEF finding, both of the PML group and Sham group actually observed a reduction in Angina class and improvement by at least one class or by at least two classes (albeit in different ratio) which the PML group can claim superiority because there were more successfully cases.
However, the author finds that there are actually different baseline characteristics in the randomized group. In other words, both of the PML group and Sham group are not segmented according to same considerable health status. For example, in the table shown on page 9 extracted from BELIEF trial, the Sham group have more patients with a history of diabetes mellitus, systemic hypertension, myocardial infarction and even the history of smoking.
Will this unbalance randomized group affect the studies? Has the unbalanced group contributed more adverse events (including 2 patients’ deaths) in the Sham group than the PML group? Looking at the all-cause mortality at 1 year with the PML group at 0% compared to the Sham group at 5%, why was the mortality rate loop sided to the advantage of the PML group.
All this are questions that the author believes is important for future similar trial. The pitfall of BELIEF trial in this aspect is that it does not explicitly answer in the finding and report. There was no mention of how professional medical personnel interview and assess each and every participating patients on their actual health condition whether they are fit to undergo the treatments.
The best practice is to design a trial that looks at each and individual health assessment in robust ways before determining the selection of the randomized group. Looking into the details of every patient are crucial in which Haynes and Haines (1998) have reported practitioner must interview and assess if the patient has any other problems that might influence the decision of clinical trial treatment. For example, patients must be physically fit enough to have invasive surgery.
EdwinNgChunPeng_RAPS_Module 2_Term Report_2015_2016 pg. 4

2.4 NOT EUROPEAN UNION (EU) AND FDA APPROVED?
In this BELIEF trial, there was no mentioned of any compliance to Clinical investigation plan (CIP). Furthermore, there was no report of the adherence of preparing the CIP in accordance with ISO 14155:2011 Clinical investigation of medical devices for human subjects – Good clinical practice.
The pitfall and omission will not ensure BELIEF trial to be compliance with EU regulation on clinical investigation of the medical device. Furthermore, Saririan and Eisenberg (2003) reported Percutaneous myocardial laser revascularization (PML) appears to be associated with less morbidity than Transmyocardial laser revascularization (TMR) but the PML technique is still considered investigational and is not FDA approved.
The author believes the design of the BELIEF trial was focused more on the device whether it is shown to be safe in bench and in vivo testing with significant clinical benefits that have received or under evaluation for European authorization. Conversely, there was lesser emphasis on fulfilling the Clinical investigation plan.
The author suggests that although Norway not a member state of the European Union (EU), it maintains membership in the European Economic Area (EEA), in the context of being a European Free Trade Association (EFTA) member.
The design of the BELIEF trial should consider consulting the EU Clinical Trials Register on the protocol prior to execution.
This is imperative as the BELIEF trial were executed, study and follow up together with medical therapy. Furthermore, EU Clinical Trials Register (No date) is an official database containing the guidelines and requirements of conducing clinical trial with investigator sites in both of the EU and or EEA.
2.5 PRIMARY MECHANISM STILL UNKNOWN?
This BELIEF trial reasoned that there were other five independently conducted, randomized controlled trials of TMR as sole therapy (1 year result) shown significantly consistent improvement in angina symptoms, quality of life, and cardiac event-free survival. As a result, the design of the BELIEF trial is perceived to be ethically allowable.
In this regard, the author does not agree that the precedent five trials are comparable on an equal footing because the design, equipment, methods and consideration are all different. Therefore, more emphasis has to be placed in the various clinical trial phases.
Especially Michael (1999) commented all Transmyocardial revascularization (TMR) have not addressed the issue of mechanism of any benefit, it can be a cause and effect of opening the channels to stay open and create a reptilian heart with sinusoids for perfusion of the myocardium and even denervation may be the mechanism.
The author suggests holding a 4 phases clinical trial namely: phase 1- test out the treatment to evaluate its safety, determine a safe dosage range and to identify side effects.
Phase 2- test out the treatment to a larger group of people to assess the effectiveness and to further evaluate its safety.
Phase 3- test out the treatment to an even larger group to confirm its effectiveness, monitor side effects, compile, compare and contrast all information to further allow the treatment to be used safely.
Phase 4- After acceptance in more countries to carry out the treatment, to gather information on the treatment effect in various populations and any side effects associated with long-term use.
EdwinNgChunPeng_RAPS_Module 2_Term Report_2015_2016 pg. 5

2.6 IS BELIEF TRIAL MORE THAN A CASE STUDY?
Kramer and Cutlip (2015) championed that pivotal studies leading to regulatory approval of high-risk cardiovascular devices should be made available in the peer-reviewed literature especially when these devices constitute practice-changing therapies.
The author also strongly agrees that it is a must to disclose and distribute as much useful information and finding as secondary data/information in order to help advanced the technique and technology on a wider global platform.
The author suspected that the BELIEF trial case study cannot be considered as a peer-reviewed literature because firstly it cannot be searched as a journal paper from various public-domain libraries resources including the National University of Singapore (NUS) library journal articles database.
Secondly, the BELIEF trial was actually a case studies published by Becker, K.M. & Whyte, J.J. (2006) in the book known as a Clinical evaluation of medical devices: principles and case studies.
Thirdly, even though the BELIEF trial case mentioned about the funding for the trial was provided through a grant from the Bergen Norway Heart Foundation and none of the treating investigators had any financial interest in the manufacturer of the investigational device. Conversely, there was no disclosure statements from the writer (Nordrehaug and Faul) to prevent any compromise arising from undeclared financial support or other benefits.
In order for practitioners to make informed clinical decisions for future similar treatment, rather than relying only on peer-reviewed literature. The author suggests any future clinical trial to be published in both of the EU Clinical Trials Register (No date) [A service of European Medicines Agency] and ClinicalTrials.gov (2015) [A service of the U.S. National Institutes of Health].
Both of this platform provides patients, their family members, health care professionals, researchers, and the public with easy access to information on publicly and privately supported clinical studies
2.7 MONETARY OR INTRINSIC MOTIVATION?
Science Letter editors (2008) reported monetary reward to participation in clinical trial study will affect their willingness to participate compared to no monetary reward. Based on the above finding, the author find the BELIEF trial not offering any form of compensation to the participating patients was not patient-friendly because since the no-option angina patients are less likely to be drawn by the financial incentives, but by offering gesture of goodwill token sum of money for participation seemed to be humanely and morally right to do so in the author point of view.
Conversely, there was no record of finding to show how many eligible patients actually opt out because of the lack of monetary compensation. This is a question worth investigating because the BELIEF trial was actually conducted in a multi-centres setting, firstly, Haukeland University Hospital (Bergen, Norway) and secondly, Ullevääl University Hospital (Oslo, Norway). Either location will require a considerable amount of time, effort, and money to travel to and return.
2.8 RIGHT VS REGULATION
The BELIEF trial is fully aware of the red-tape and acted diligently in complying with the regulation needs. No doubt it had complied with the various regulation and ethical bodies. Furthermore, it was perceived to be successfully in term of the design and conduct of the trial, there was no major error in term of randomization, concealment, and blinding and data collection.
However, the author would like to see from the perspective of the Sham group. The glaring point from the BELIEF trial was that patients were only notified of their randomized assignments into PML group and Sham group after the 1-year follow-up. The author believes the higher purpose of the BELIEF trial is to investigate the “right treatment” for the no-option angina patients.
EdwinNgChunPeng_RAPS_Module 2_Term Report_2015_2016 pg. 6

On the other hand, the author strongly argues that the Sham group have every right to be exposed to “real” treatment same as what the PML group of patients received. Therefore to address this pitfall, the author recommends the BELIEF trial to be designed as a cross-over type, allowing both PML group and Sham group to be assessed from the two aspects. By allowing cross-over, both of the PML group and Sham group will not be denied the right to be treated.
On the other hand, Bridges, et al. (2006) reported severity angina patients with only sole-therapy PML treatment experience early morbidity, the author believes that the BELIEF trial should have also taken care of the patient’s drug management seriously because there were no dose changes in any cardiovascular medication through the 1 year. Was it by design or by situation?
2.9 MAN VS WOMEN
In this BELIEF trial, there were only 2 women (5%) in the PML group and 5 women (12%) in the Sham group.
The author believed the ratio is not proportionally distributed to run the trial as man and women have different epidemiological characteristics. Redberg and Dhruva (2012) goes to the extent to report that women have higher procedural morbidity and mortality than men during many invasive medical devices procedures.
In order to overcome this pitfall and to further investigate the effects of gender-specific safety and effectiveness assessment, the author suggests designing clinical trials that focus on men only or women only or equal sample size between man and women.
2.9.1 PLACEBO EFFECT ON BOTH PLACEBO AND NON-PLACEBO GROUP
As noted by Nordrehaug and Fauls (1996) the BELIEF clinical trial was designed as a randomized, two-arms, double-blind clinical trial to control for patient bias (the placebo effect) and investigator bias in determining the clinical benefit of Percutaneous Myocardial Laser (PML) treatment.
Credit must be given to Nordrehaug and Fauls for designing a trial to consider and covered all possible angle to control for patient bias (the placebo effect). This sentiment was also echoed by Howick (2008) who concluded that keeping trials successfully double-masked is extremely difficult.
Conversely, there is no perfect fool proof plan. Roy (2012) argues any patient receiving an active treatment might also have falsely believe that they are receiving the placebo or Sham therapy. Granger and Gersh (2015) also argues that even when the patients have been effectively kept unaware of the study assignment, both of the placebo and non-placebo group patients still would believe that they have received the same active treatment.
Bonetti, et al. (2003) commented that the mechanism of action of PML laser therapy in most multiple randomized trials have failed to demonstrate an increase in survival and most of the trial are not fully able to explain the placebo effect. Further and longer-term trial and research are needed to elucidate the value of PML treatment. In conclusion, there may not be 100% control for patient bias among the PML group and Sham group!
Upholding all of the above argument, the author strongly agrees that the placebo effect would also have influence patients who are receiving the active treatment to lead to more “feel good” effect and that may explain the improvement in Canadian Cardiovascular Society grading (CCS) angina class for the PML group as compared to the Sham group.
A longer study with cross over of patients will be crucial to address the above pitfalls. There is also a need to look beyond the one-year clinical benefits so as to assess the patient’s after-treatment holistically. The author suggests for future similar trial to have a post-assessment check-up for the patients every year for a five years recording periods.
EdwinNgChunPeng_RAPS_Module 2_Term Report_2015_2016 pg. 7

2.9.2 INFORMED CONSENT = INFORMED RISK?
The BELIEF trial reported that patients were issues with written informed consent prior to the treatment. Despite advances in PML treatment and patient management, the author believes any identified risk must be fully disclosed to the patient, on top of written informed consent, any associated risks have to be communicated to the patients. Robinson and Cook (2006) champion that the highest priority in any clinical trial is the protection of research subjects and patients from any injury.
As a result, the author believes the BELIEF clinical trial design should be focusing more on the risk management for the investigational device that consists of two catheters dual system and its limitation during the clinical application that will still allow laser energy to continue to penetrate the tissue to a depth of around 5 to 6cm.
The risk management finding, limitation, control methods and the reason for requiring patients to have at least 8 mm thick of the left ventricular wall so as to reduce the potential for pericardial perforation have to be clearly communicated to patients on top of the necessary informed consent.
The author suggests the BELIEF to implement the EN ISO 14971 Risk Management for Medical Devices and ICH Harmonised Tripartite Guideline Q9 for Quality Risk Management both for clinical trial risk management. This is important because throughout this BELIEF trial, only one individual participating in the procedures, the laser operator, was aware of the randomized assignments.
In the author point of view, there was no 2nd opinion, supervision, and control while the laser operator acted to power on or power off the lead box that transmits laser after reading the treatment assignment envelope. There are many possible risk factors such as mix-up of the envelope, misinterpretation of the envelope content, simple human-prone mistake by pressing/executing wrongly and even act of sabotaging and many others issues.
3.0 CONCLUSION BY THE AUTHOR
The author would like to conclude this term paper by discussing on the suitability, feasibility and acceptability factors of the BELIEF trial. As in the real world, there will never be a silver bullet to solve every single problem.
The key point is to assess all available options on the table and do a weightage between the risks and benefits to come up with a decision for the greater good for the patients, stakeholders and industry.
3.1 SUITABILITY (WOULD IT WORK?)
The BELIEF trial would not have existed but because of the promising results from the previous animal testing. Huges, et al. (2002) reported prior to the year 2002, six prospective randomized animal TMR controlled trials have demonstrated the efficacy of surgical TMR for decreasing anginal symptoms in patients ineligible for traditional methods of revascularization.
In term of suitability, the many extensive data collected from animal testing, bench testing and in vitro studies have identified the suitability to be practiced on a human subject. The hard question is to identify, qualifies and characterize the actual mechanisms of action which is still an never ending work in progress.
3.2 FEASIBILITY (CAN IT BE MADE TO WORK?)
There will be many unforeseen circumstances that lead to more questions than answer. Therefore, there will always be trial and errors while conducting any clinical trial, the author believes that the utmost important task is to prevent and reduce injury and harm to the participating patients.
By designing a robust clinical trial with the mind and concern of patient’s safety first is definitely the right approach. Stone, et al. (2015) reported the primary and secondary endpoints should be selected such that
EdwinNgChunPeng_RAPS_Module 2_Term Report_2015_2016 pg. 8

meeting these endpoints will demonstrate reasonable assurance of safety and effectiveness and a favorable benefit-risk profile.
The design of any clinical trial should, therefore, be focusing first on the feasibility of going through the safest ways (no short-cut) to achieve the primary and secondary endpoints objectives.
3.3 ACCEPTABILITY (WILL THEY WORK IT?)
The author believes there will be consensus effort among the various stakeholders to work on and fine-tune any similar BELIEF trial in the future because until now, the no options patients are still without any real options. Leon, et al. (2005) reported the patients studied in these similar BELIEF trials had severe angina symptoms who had exhausted all forms of conventional therapy.
They were highly motivated and desperate for a novel therapy to provide symptom relief, and they had high expectations for clinical benefit. Therefore the author strongly advocate more research to be carry out in the field of Percutaneous Myocardial Laser Therapy to discover more finding and revealing the side-effects so as to allow more research fellow, professional medical personnel and suffering patients to see the pro and con before accepting the Percutaneous Myocardial Laser Therapy as a suitable, feasible and acceptable long-term treatment.
End of Report
EdwinNgChunPeng_RAPS_Module 2_Term Report_2015_2016 pg. 9

REFERENCES
Bridges, C.R., Horvath, K.A., Chiu, R.C. & Wiley InterScience (Online service) (2006) Myocardial laser revascularization. Blackwell Futura, Malden, Mass.
Bonetti, P.O., Holmes, D.R., Lerman, A. & Barsness, G.W. (2003) Enhanced external counterpulsation for ischemic heart disease: Placebo effect of myocardial laser revascularization is important. Journal of the American College of Cardiology, vol. 41, no. 11, pp. 1918-1925.
Becker, K.M. & Whyte, J.J. (2006) Clinical evaluation of medical devices: principles and case studies, 2nd edn, Humana Press, Totowa, N.J.
Cooper, C., O'Cathain, A., Hind, D., Adamson, J., Lawton, J. & Baird, W. (2014) Conducting qualitative research within Clinical Trials Units: avoiding potential pitfalls. Contemporary clinical trials, vol. 38, no. 2, pp. 338-343.
Granger, C.B. & Gersh, B.J. (2015) Potential relief for refractory angina. The New England journal of medicine, vol. 372, no. 6, pp. 566-567.
Galiñanes, M., Loubani, M., Sensky, P.R., Hassouna, A., Cherryman, G.R., Leverment, J.N. & Samani, N.J. (2004) Efficacy of transmyocardial laser revascularization and thoracic sympathectomy for the treatment of refractory angina. The Annals of Thoracic Surgery, vol. 78, no. 1, pp. 122-128.
Howick, J. (2008) Double-Blinding: The Benefits and Risks of Being in the Dark. In Fennell, D. (editors). Centre for the Philosophy of Natural; and Social Science Contingency and Dissent in Science Technical Report. (03/08). London, The London School of Economics and Political Science.
Haynes, B. & Haines, A. (1998) Getting research findings into practice: Barriers and bridges to evidence based clincial practice. British Medical Journal, vol. 317, no. 7153, pp. 273.
Hughes, G.C., Biswas, S.S., Yin, B., Baklanov, D.V., Annex, B.H., Coleman, R.E., DeGrado, T.R., Landolfo, K.P., Landolfo, C.K. & Lowe, J.E. (2002) A comparison of mechanical and laser transmyocardial revascularization for induction of angiogenesis and arteriogenesis in chronically ischemic myocardium. Journal of the American College of Cardiology, vol. 39, no. 7, pp. 1220-1228.
Kramer, D.B. & Cutlip, D.E. (2015) Trust and transparency in clinical trials of medical devices. Nature Reviews Cardiology, vol. 12, no. 9, pp. 503.
Leon, M.B., Kornowski, R., Downey, W.E., Weisz, G., Baim, D.S., Bonow, R.O., Hendel, R.C., Cohen, D.J., Gervino, E., Laham, R., Lembo, N.J., Moses, J.W. & Kuntz, R.E. (2005) A Blinded, Randomized, Placebo-Controlled Trial of Percutaneous Laser Myocardial Revascularization to Improve Angina Symptoms in Patients With Severe Coronary Disease. Journal of the American College of Cardiology, vol. 46, no. 10, pp. 1812-1819.
Michael, H. Crawford. (1999) TMR Revisited. Clinical Cardiology Alert, vol. 18, no. 11, pp. 81.
Nordrehaug, J.E. & Fauls, J.M. (1999) BELIEF: A randomized, Sham-procedure-controlled trial of Percutaneous Myocardial laser therapy. In Becker, K.M. & Whyte, J.J. (editors). Clinical evaluation of medical devices : principles and case studies. (2nd edition) (2006). Totowa, NJ: Humana Press Inc.
EdwinNgChunPeng_RAPS_Module 2_Term Report_2015_2016 pg. 10

Robinson, M. & Cook, S. (2006) Clinical trials risk management. CRC/Taylor & Francis, Boca Raton.
Roy, J. (2012) Randomized treatment-belief trials. Contemporary Clinical Trials. 33. pp.172-177.
Redberg, R.F. & Dhruva, S.S. (2012) Evaluating Sex Differences in Medical Device Clinical Trials: Time for Action. JAMA, vol. 307, no. 11, pp. 1145-1146.
Science Letter editors. (2008) Clinical Trial Participation Unaffected by Disclosure of Investigator's Financial Stake. Food and Drug Law Journal Article Finds 2008, , NewsRX LLC, pp. 292.
Stone, G.W., Vahanian, A.S., Adams, D.H., Abraham, W.T., Borer, J.S., Bax, J.J., Schofer, J., Cutlip, D.E., Krucoff, M.W., Blackstone, E.H., Généreux, P., Mack, M.J., Siegel, R.J., Grayburn, P.A., Enriquez-Sarano, M., Lancellotti, P., Filippatos, G., Kappetein, A.P. & Mitral Valve Academic Research Consortium (MVARC) (2015) Clinical Trial Design Principles and Endpoint Definitions for Transcatheter Mitral Valve Repair and Replacement: Part 1: Clinical Trial Design Principles: A Consensus Document From the Mitral Valve Academic Research Consortium, Journal of the American College of Cardiology, vol. 66, no. 3, pp. 278.
Saririan, M. & Eisenberg, M.J. (2003) Myocardial laser revascularization for the treatment of end-stage coronary artery disease, Journal of the American College of Cardiology, vol. 41, no. 2, pp. 173-183.
The EU Clinical Trials Register (No date) About the EU Clinical Trials Register. Available at: https://www.clinicaltrialsregister.eu/about.html (Accessed: 21 Feb 2016). ClinicalTrials.gov (2015) Background of ClinicalTrials.gov. Available at: https://clinicaltrials.gov/ct2/about-site/background (Accessed: 21 Feb 2016).
<End of References>
EdwinNgChunPeng_RAPS_Module 2_Term Report_2015_2016 pg. 11