A stepwise surgical procedure to investigate the lymphatic transport of lipid-based oral drug...
-
Upload
michael-boyd -
Category
Documents
-
view
212 -
download
0
Transcript of A stepwise surgical procedure to investigate the lymphatic transport of lipid-based oral drug...

www.elsevier.com/locate/jpharmtox
Journal of Pharmacological and Toxicological Methods 49 (2004) 115–120
Original article
A stepwise surgical procedure to investigate the lymphatic transport of
lipid-based oral drug formulations: Cannulation of the mesenteric and
thoracic lymph ducts within the rat
Michael Boyda, Verica Risovicb, Philip Julla, Eugene Choob, Kishor M. Wasanb,*
aAcute Care Animal Unit, Koerner Pavilion, University of British Columbia, Vancouver, BC, CanadabDivision of Pharmaceutics and Biopharmaceutics, Faculty of Pharmaceutical Sciences, University of British Columbia, 2146 East Mall Avenue,
Vancouver, BC, Canada V6T 1Z3
Received 8 September 2003; accepted 24 November 2003
Abstract
Introduction: A number of animal models have been described for the assessment of intestinal lymphatic drug transport. Lymphatic
transport studies are commonly first conducted in the laboratory rat, with larger more complicated models (i.e., dog or pig) subsequently
investigated. However, the utility of lymph fistulation in large animals is limited by considerable logistical and economic constraints.
Methods: This paper describes a stepwise surgical procedure for cannulating the thoracic and mesenteric lymph ducts in male Sprague–
Dawley rats. Results: Following surgery, thoracic and mesenteric lymph flow rates during the 24-h period immediately following surgery
averaged 12.5F 2.5 and 2.4F 1.1 ml/h, respectively. This flow rate is greater than that obtained with previously described methods, which
require restraint of the animals and/or a 24-h recovery period and are reported to produce average intestinal lymph flow rates of 2 ml/h.
Discussion: This animal model can be utilized for the assessment of drug transport by the lymphatics and for determining what percentage of
lymphatic transport is a result of only intestinal lymphatics.
D 2004 Elsevier Inc. All rights reserved.
Keywords: Mesenteric lymph duct; Thoracic lymph duct; Rat; Surgical procedure; Lymphatic drug delivery
1. Introduction ing general systemic drug exposure (Porter & Charman,
The gastrointestinal lymphatic system is a specific trans-
port pathway through which dietary lipids (Borgstrom,
Dahlqvist, Lundh, & Sjoval, 1957; Shiau, 1981; Thomson,
Keelen, Garg, & Clandinin, 1989; Thomson, Schoeller,
Keelen, Smith, & Clandinin, 1993), fat-soluble vitamins,
and water-insoluble compounds (i.e., halofantrine, ontazo-
last, amphotericin B) can gain access to the systemic circu-
lation (Hauss et al., 1998; Holm, Porter, Mullertz,
Kristensen, & Charman, 2002; Porter & Charman, 2001;
Wasan, 2002). Drugs transported by way of the gastrointes-
tinal lymphatic system bypass the liver and avoid potential
hepatic first-pass metabolism. Lymphatic delivery of immu-
nomodulatory agents and low therapeutic index drugs used
in the treatment of cancer cell metastases and HIV present an
opportunity to maximize therapeutic benefit while minimiz-
1056-8719/$ – see front matter D 2004 Elsevier Inc. All rights reserved.
doi:10.1016/j.vascn.2003.11.004
* Corresponding author. Tel.: +1-604-822-4889; fax: +1-604-822-
3035.
E-mail address: [email protected] (K.M. Wasan).
2001; Tucker, 1993). Furthermore, lymphatic drug transport
may promote drug incorporation into the body’s lipid-han-
dling system, thus offering the potential to manipulate drug
distribution and residence time within the body.
The majority of orally administered drugs gain access to
the systemic circulation by direct absorption into the portal
blood (Porter & Charman, 2001;Wasan, 2002). However, for
some water-insoluble compounds, transport by way of the
intestinal lymphatic system may provide an additional route
of access to the systemic circulation (Porter & Charman,
2001; Wasan, 2002). Exogenous compounds absorbed
through the intestinal lymph appear to be generally trans-
ported in association with the lipid core of intestinal lip-
oproteins (predominantly triglyceride-rich chylomicrons),
thereby requiring coadministered lipid to stimulate lipopro-
tein formation. Delivery into the bloodstream by way of the
intestinal lymphatics has been suspected to contribute to the
overall absorption of a number of highly lipophilic com-
pounds (Adachi, Liu, Horkoshi, & Ueno, 1993; Barnwell et
al., 1992; Gallo-Torres, 1970; Hauss, Mehta, & Radebaugh,

M. Boyd et al. / Journal of Pharmacological and Toxicological Methods 49 (2004) 115–120116
1994; Horst et al., 1976; Sugihara & Furuuchi, 1988; Sugi-
hara, Furuuchi, Ando, Takashima, & Harigaya, 1988), in-
cluding cyclosporine (Ueda, Lemaire, Gsell, & Nussbaumer,
1983), naftifine (Grimus & Schuster, 1984), probucol (Palin
&Wilson, 1984), mepitiostane (Ichihashi, Kinoshita, Shima-
mura, & Yamada, 1991; Ichihashi, Kinoshita, Takagishi, &
Yamada, 1991; Ichihashi, Kinoshita, Takagishi, & Yamada,
1992a; Ichihashi, Kinoshita, Takagishi, & Yamada, 1992b;
Ichihashi, Kinoshita, & Yamada, 1991), halofantrine (Holm
et al., 2002; Humberstone, Porter, & Charman, 1996; Porter,
Charman, & Charman, 1996; Wasan et al., 1999), and poly-
chlorinated biphenyls (Busbee, Yoo, Norman, & Joe, 1985).
Lymph from the intestinal lymphatic system (as well as
hepatic and lumbar lymph) drains through the thoracic lymph
duct into the left internal jugular vein and then to the systemic
circulation (Davidson, 1994; Johnson, 1976; Tso, 1994).
Thus, the transport of drug by way of the intestinal lymphatic
system may increase the percentage of drug that can gain
access to the systemic circulation. In addition, the process of
intestinal lymphatic drug transport often continues over time
periods longer than typically observed for drug absorption
through the portal vein. Consequently, drug transport
through the lymph may be utilized to prolong the time course
of drug delivery to the systemic circulation.
A number of animal models have been described for the
assessment of intestinal lymphatic drug transport (Charman
& Porter, 1996; Porter & Charman, 1997; Porter & Charman,
2001; White, Story, & Barnwell, 1991). Lymphatic transport
studies are commonly first conducted in the laboratory rat,
with larger more complicated models (i.e., dog or pig)
subsequently investigated (Charman & Porter, 1996; Porter
& Charman, 1997; Porter & Charman, 2001; White et al.,
1991). However, the utility of lymph fistulation in large
animals is limited by considerable logistical and economic
constraints. Ideally, sampling strategies for lymphatic trans-
port studies should provide the capacity to estimate both the
extent of lymphatic transport, as well as the extent of portal
blood absorption in order to estimate the overall bioavail-
ability of the drug/formulation. This strategy enables the
unambiguous determination of the extent of lymphatic
transport, relative to absorption via the portal blood, and
the total bioavailability of the drug/formulation. As lymphat-
ic transport can be affected by experimental factors such as
the site of lymphatic cannulation the period of fasting prior to
dosing (Charman & Porter, 1996; Kararli, 1995; Levet-
Trafit, Gruyer, Marjanovic, & Chou, 1996; Liu, Adachi,
Horkoshi, & Ueno, 1995; Porter & Charman, 1997; Porter &
Charman, 2001; White et al., 1991), it is important to
standardize procedures when comparing between studies.
Previously reported methods for collecting lymph from
the rat required total restraint of the animal and fluid
replacement, by intravenous or intraduodenal infusion, to
maintain lymph output (Carey, Small, & Bliss, 1983; Chang
& Bodmeier, 1997; Shah, Carvajal, Patel, Infeld, & Malick,
1994). Hauss, Fogal, and Ficorilli (1998) have developed a
rat model to allow collection of mesenteric lymph for 5 days
from conscious, minimally restrained animals with fully
patent cannulae and no signs of physical distress. This
model obviates the need for total restraint or general
anesthesia, both of which are known to influence intestinal
lymphatic transport of test compounds in unpredictable
ways. Animals were provided free access to an electrolyte
solution, which they consume in sufficient quantity to
maintain adequate lymph output without the need for the
previously required infusions for fluid replacement. How-
ever, the main limitation of this model is that both the
thoracic lymph duct and mesenteric lymph duct could not be
cannulated simultaneously.
The triple cannulated anaesthetized rat model (where the
mesenteric lymph duct, jugular vein, and duodenum are
accessed) has been used for the assessment of lymphatic
transport. General anesthesia precludes oral dosing in the
anaesthetized model, and consequently drug and lipid for-
mulations are administered intraduodenally (Charman &
Porter, 1996; Porter & Charman, 1997; Porter & Charman,
2001; White et al., 1991). This limitation thus circumvents
the inherent emulsifying action of the stomach and the
potential effects of lipids on gastric emptying. Thus, the
conscious rat model best represents the in vivo situation in
terms of both lack of anaesthetic effects and the ability to
orally administer drug formulations. In addition, in this
model both the thoracic lymph duct and mesenteric lymph
duct could not be cannulated simultaneously.
This paper describes the development of a cannulated rat
model, where both the thoracic and mesenteric lymph ducts
are accessed simultaneously for the assessment of drug
transport by the lymphatics and what percentage of lym-
phatic transport is a result of only intestinal lymphatics.
2. Methods
The animals were cared for in accordance with the
principles and guidelines of the Canadian Council on Animal
Care (CCAC). Male Sprague–Dawley rats (Charles River,
Montreal, Canada), 350–375 g in weight, were used for all
surgical procedures. The rat is the appropriate experimental
animal to investigate oral absorption and lymphatic transport
because intestinal characteristics (i.e., anatomical, metabolic,
and biochemical characteristics) of these animals are similar
to those found in humans (Fagerholm, Johansson, & Len-
nermas, 1996; Kararli, 1995; Levet-Trafit et al., 1996; Soria
& Zimmerman, 1996). Specifically, the intestinal processing
and absorption of dietary lipids are similar in rats and
humans (Pahl, Oveisi, Khamiseh, & Vaziri, 1998).
2.1. Surgical procedures
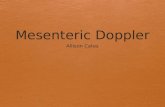
2.1.1. Mesenteric lymph duct cannulation (Fig. 1)
1. One hour preoperatively, the rat was given 1.5–2 ml of
olive oil by oral gavage for a 350- to 375-g rat.

M. Boyd et al. / Journal of Pharmacological and Toxicological Methods 49 (2004) 115–120 117
2. The rat was given 0.03–0.05 mg/kg atropine subcuta-
neously 20 min prior to surgery.
3. Induction of anesthesia was achieved with a 1-l oxygen
flow containing 5% isoflurane in a chamber.
4. The rat was transferred to a nose cone and a 2%
isoflurane solution with a 1-l oxygen flow was used to
maintain anesthesia during surgery.
5. Intravenous access was achieved using a 25-g butterfly
into the right tail vein. The butterfly was attached to a
60 drops/ml intravenous solution set and a 50-ml 0.09%
saline bag.
6. The rat was positioned in dorsal recumbency and hair
was clipped from the manubrium to the femoral area.
7. Upon removal of the hair, ophthalmic ointment was
applied generously to the eyes.
8. A three-step surgical scrub was preformed on the shaven
sites:
(a) First, the shaven sites are cleaned with a 0.5% P/V
chlorhexidine alcohol-based solution.
(b) Second, Betadine surgical scrub solution were ap-
plied with a clean 4� 4 in ever-increasing circles
away from midline. The removal of the scrub
solution follows a similar pattern with a sterile 4� 4.
(c) Third, the shaven areas were painted with a generous
layer of Betadine Solution.
9. A midline abdominal incision was made approximately
two thirds of the length of the abdomen posterior to the
xiphoid cartilage.
10. The intestine was brought out and wrapped in gauze that
has been soaked in warm saline.
11. The intestine was placed on the right side of the abdomen.
This exposes the posterior vena cava and the left renal
vein.
12. The mesenteric lymph duct was seen in the mesentery as
a white duct accompanying the mesenteric artery (see
Fig. 1). Both are attached with connective tissue.
13. Slight tension was placed on the duct and artery using
cotton tipped applicators, mall probes, and iris forceps.
Fig. 1. Retracted mesenteric lymphatic duct.
14. The connective tissue around the duct and artery was
cleared. A length of approximately 10 mm was suffi-
cient for cannulation.
15. When separated, vessel loops are placed around the
artery for retraction.
16. Two 4-0 silk ligatures are placed around the duct.
17. A 15-cm length of polyethylene tubing (id 0.58 mm, od
0.965 mm) was cut at one end diagonally to produce a
beveled point.
18. The tubing was primed with heparinized saline (20 units
heparin per ml). A syringe filled with heparinized saline
was left attached to the tubing.
19. A 16-G catheter was tunneled under the vena cava at the
point of angle that the lymph duct makes with the vena
cava. The catheter should be parallel and on top of the
duct.
20. The tubing was passed through the catheter and the
beveled tip is placed in position with the duct.
21. The catheter was removed.
22. To facilitate placement of the tubing into the duct, an
introducer was shaved at the tip to produce a more
obtuse angle and sharper tip.
23. Using the silk ties, gentle tension was applied and the
introducer was used to puncture the duct. With the
introducer in place, the tip of the tubing was slid into
the duct approximately 5 mm.
24. The syringe was detached from the tubing. Small drops
of heparinized saline are produced on the end of the
tubing as the lymph replaces the saline in the tubing.
25. Silk ligatures are tied down to secure tubing. Lymph
flow was seen from as a white solution in the tubing. If
a proper seal cannot be achieved with the ties, tissue
adhesive may be applied over the ligatures.
26. Warm saline was used to moisten the intestine and
abdominal cavity. The intestine was replaced in the
normal position.
27. Using continuous suturing, the peritoneum was closed
with a 4-0 vicryl taper needle. The skin was closed with
interrupted mattress sutures using a 4-0 vicryl cutting
needle.
28. Topical anesthetic cream was applied to the suture line
on the rat. Temgesic (buprenorphine, Schering-Plough)
was administered subcutaneously in the dose of 0.01–
0.05 mg/kg. This drug is commonly used immediately
after surgery to relieve pain associated with the surgery.
Emla cream (lidocaine 2.5% and prilocaine 2.5%) was
used topically to prevent itching. The rat was revived on
1 l oxygen and 0% isoflurane.
29. Oral gavage was preformed to administer the drug.
30. The rat remains warm in dorsal recumbency and kept
warm with IV fluids to promote good lymph flow.
Animals were under slight isoflurane anesthesia (1 l
oxygen flow containing 0.25% of isoflurane solution)
during lymph collection for 6–8 h.
31. Upon completion of lymph collection (6–8 h), 5 ml of
blood was collected by cardiac puncture and the rat was

Fig. 2. Cannulated thoracic lymphatic duct.
Fig. 3. Postoperation cannulated animal set-up.
M. Boyd et al. / Journal of Pharmacological and Toxicological Methods 49 (2004) 115–120118
euthanized with sodium pentobarbitol 120 mg/kg iv.
The right kidney, spleen, liver, heart, and lungs were
harvested.
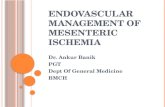
2.1.2. Thoracic lymph duct cannulation (Fig. 2)
1. A 15-cm length of polyethylene tubing (id 0.58 mm, od
0.965 mm) was curved at one end by passing a bent wire
through it and plunging the curved end in boiling water
to produce a 2-cm end bent 160 relative to the rest of the
tubing. The tubing the gas sterilized (Fig. 2).
2. One hour preoperatively, the rat was given 1.5–2 ml of
olive oil by oral gavage for a 350- to 375-g rat.
3. The rat was given 0.03–0.05 mg/kg atropine subcuta-
neously 20 min prior to surgery.
4. Induction of anesthesia was achieved with a 1-l oxygen
flow containing 5% isoflurane in a chamber.
5. The rat was transferred to a nose cone, and a 2%
isoflurane solution with a 1-l oxygen flow was used to
maintain anesthesia during surgery.
6. Intravenous access was achieved using a 25-g butterfly
into the right tail vein. The butterfly was attached to a
60 drops/ml iv solution set and a 50 ml 0.09% saline
bag.
7. The rat was positioned in dorsal recumbency and hair
was clipped from the manubrium to the femoral area.
8. Upon removal of the hair, ophthalmic ointment was
applied generously to the eyes.
9. A three-step surgical scrub was preformed on the shaven
sites:
(a) First, the shaven sites were cleaned with a 0.5% P/V
chlorhexidine alcohol-based solution.
(b) Second, Betadine surgical scrub solution was applied
with a clean 4� 4 in ever increasing circles away
from midline. The removal of the scrub solution
follows a similar pattern with a sterile 4� 4.
(c) Third, the shaven areas were painted with a generous
layer of Betadine Solution.
10. A midline abdominal incision was made approximately
two thirds of the length of the abdomen posterior to the
xiphoid cartilage.
11. The intestine was brought out and wrapped in gauze that
has been soaked in warm saline.
12. The left kidney and adrenal were separated from the
connective tissue and fat. Together, kidney, adrenal, in-
testine, stomach, and spleenwere wrapped in warm saline
soaked gauze and retracted to the right side of the rat.
13. The thoracic lymph duct, lying parallel and partially
underneath the abdominal aorta, was separated away
from the vessel by applying slight pressure to the aorta
and gently teasing away connective tissue.
14. Vessel loops were placed around the abdominal aorta for
retraction.
15. Two 4-0 silk ligatures were placed around the lymph
duct.
16. The 15-cm length of polyethylene tubing was cut at the
bent end diagonally to produce a beveled point.
17. The tubing was primed with heparinized saline (20 units
heparin per ml). A syringe filled with heparinized saline
was left attached to the tubing.
18. A 16-G catheter was tunneled through the peritoneum
and skin in the lower left quadrant.
19. The tubing was passed through the catheter and the
beveled tip is placed in position with the duct.
20. The catheter was removed leaving the polyethylene
tubing in place.
21. To facilitate placement of the tubing into the duct, an
introducer was shaved at the tip to produce a more
obtuse angle and sharper tip.
22. Using the silk ties, gentle tension is applied and the
introducer was used to puncture the duct. With the
introducer in place, the tip of the tubing was slid into
the duct approximately 5 mm.
23. Silk ligatures were tied down to secure tubing. Lymph
flow was seen as a white solution in the tubing. If a

Fig. 4. Mesenteric lymphatic duct branches in 45% of Sprague–Dawley
rats used.
M. Boyd et al. / Journal of Pharmacological and Toxicological Methods 49 (2004) 115–120 119
proper seal cannot be achieved with the ties, tissue
adhesive may be applied over the ligatures.
24. The syringe was detached from the tubing. Small drops
of heparinized saline were produced on the end of the
tubing as the lymph replaces the saline in the tubing.
25. Warm saline was used to moisten the intestine and
abdominal cavity.
26. The intestine was replaced in the normal position. Using
continuous suturing, the peritoneumwas closed with a 4-
0 vicryl taper needle. The skin was closed with inter-
rupted mattress sutures using a 4-0 vicryl cutting needle.
27. Topical anesthetic cream was applied to the suture line
on the rat.
28. The rat was revived on 1 l oxygen and 0% isoflurane.
29. Oral gavage was preformed to administer the drug.
30. The rat remains warm in dorsal recumbency and kept
warm with IV fluids to promote good lymph flow.
31. Upon completion of lymph collection (6–8 h), 5 ml of
blood was collected by cardiac puncture and the rat was
euthanized with sodium pentobarbitol 120 mg/kg iv.
The right kidney, spleen, liver, heart, and lungs were
harvested (Fig. 3).
For both the mesenteric and thoracic surgical procedures,
the following information should be noted:
(a) The exteriorized cannula was placed underneath the
sterilized gauze.
(b) The two procedures (thoracic and mesenteric) were
initially carried out in different rats (to establish each
technique). However, several rats were done where both
the mesenteric and thoracic ducts were cannulated at the
same time.
(c) The animals were housed two per cage on a 12:12-h
light/dark schedule and given food (Purina lab chow)
and water ad libitum. Upon arrival, all animals were
allowed to acclimatize in their new surroundings for 10
days prior to surgery.
(d) Animals were under slight isoflurane anesthesia (1 l
oxygen flow containing 0.25% of isoflurane solution)
during lymph collection. In these initial studies, the
animals were not manually restrained or tethered using
a dual/multichanneled swivel mechanism.
3. Results and discussion
Following surgery, thoracic and mesenteric lymph flow
rates during the 24-h period immediately following surgery
averaged 12.5F 2.5 and 2.4F 1.1 ml/h, respectively. This
flow rate is greater than that obtained with previously
described methods, which require restraint of the animals
and/or a 24-h recovery period and are reported to produce
average intestinal lymph flow rates of 2 ml/h.
The use of our modified lymph model and the described
procedures, a skilled animal surgeon can expect a success rate
of approximately 80%. The main reasons for failure of the
model are dislodged, leaking, or improperly placed cannulae.
A dislodged or leaking cannula is suspected when the lymph
flow out of the animal is sluggish; but when the cannula is
raised, the lymph flows readily back into the animal. Another
issue not mentioned in previous research (Hauss, Fogal, &
Ficorilli, 1998; Hauss et al., 1998) is the physiology of the
mesenteric lymph duct. In approximately 45% of the rats
used in this study, the mesenteric lymph duct was multiply
branched making it next to impossible to cannulate it (Fig. 4).
This is the case for not only Sprague–Dawley rats but also
Long–Evans and Wistar rats (data not shown). This physio-
logic inconsistency is one limitation to this model, and
scientists should be aware of when initiating this surgical
procedure.
In conclusion, cannulation of the thoracic and mesenteric
lymph ducts within the rat has been successfully developed
for the assessment of drug transport through the lymphatics.
This model could be utilized to evaluate the role of
lymphatics in assessing the bioavailability of drugs
incorporated into novel lipid-based formulations.
Acknowledgements
This study was supported with an operating grant from
the Canadian Institutes of Health Research (Grant #MOP-
49432 to KMW).
References
Adachi, I., Liu, H., Horkoshi, I., & Ueno, M. (1993). Possibility of lym-
phatic absorption of epidermal growth factor from intestine. Yakugaku
Zasshi, 113, 256–263.
Barnwell, S. G., Laudanski, T., Story, M. J., Mallinson, C. B., Harris, R. J.,
Cole, S. K., Keating, M., & Attwood, D. (1992). Improved oral bio-
availability of propranolol in healthy human volunteers using a liver
bypass drug delivery system containing oleic acid. International Jour-
nal of Pharmaceutics, 88, 423–432.

M. Boyd et al. / Journal of Pharmacological and Toxicological Methods 49 (2004) 115–120120
Borgstrom, B., Dahlqvist, A., Lundh, G., & Sjovall, J. (1957). Studies of
intestinal digestion and absorption in the human. Journal of Clinical
Investigation, 36, 1121–1136.
Busbee, D. L., Yoo, J. -S. H., Norman, J. O., & Joe, C. O. (1985). Poly-
chlorinated biphenyl uptake and transport by lymph and plasma com-
ponents. Proceedings of the Society for Experimental Biology and
Medicine, 179, 116–122.
Carey, M. C., Small, D. M., & Bliss, C. M. (1983). Lipid digestion and
absorption. Annual Review of Physiology, 45, 651–677.
Chang, C. M., & Bodmeier, R. (1997). Binding of drugs to monoglyceride-
based drug delivery systems. International Journal of Pharmaceutics,
147, 135–142.
Charman, W. N., & Porter, C. J. H. (1996). Lipophilic prodrugs designed
for intestinal lymphatic transport. Advanced Drug Delivery Reviews, 19,
149–169.
Davidson, N. O. (1994). Cellular and molecular mechanisms of small in-
testinal lipid transport. In L. R. Johnson (Ed.), Physiology of the gastro-
intestinal tract (3rd ed.) (pp. 1909–1934). New York: Raven Press.
Fagerholm, U., Johansson, M., & Lennernas, H. (1996). Comparison bet-
ween permeability coefficients in rat and human jejunum. Pharmaceu-
tical Research, 13, 1336–1342.
Gallo-Torres, H. E. (1970). Intestinal absorption and lymphatic transport of
d-1,3,4-3H2-alpha-tocopheryl nicotinate in the rat. International Jour-
nal for Vitamin and Nutrition Research, 40, 505–514.
Grimus, R. C., & Schuster, I. (1984). The role of the lymphatic transport in
the enteral absorption of naftifine by the rat. Xenobiotica, 14, 287–294.
Hauss, D. J., Fogal, S. E., & Ficorilli, J. V. (1998). Chronic collection of
mesenteric lymph from conscious, tethered rats. Contemporary Topics
in Laboratory Animal Science, 37, 56–58.
Hauss, D. J., Fogal, S. E., Ficorilli, J. V., Price, C. A., Roy, T., Jayaraj, A.
A., & Keirns, J. J. (1998). Lipid-based delivery systems for improving
the bioavailability and lymphatic transport of a poorly water-soluble
LTB4 inhibitor. Journal of Pharmaceutical Sciences, 87, 165–169.
Hauss, D. J., Mehta, S., & Radebaugh, G. W. (1994). Targeted lymphatic
transport and modified systemic distribution of CI-976, a lipophilic
lipid-regulator drug, via a formulation approach. International Journal
of Pharmaceutics, 108, 85–93.
Holm, R., Porter, C. J., Mullertz, A., Kristensen, H. G., & Charman, W. N.
(2002). Structured triglycerides vehicles for oral delivery of halofan-
trine: Examination of intestinal lymphatic transport and bioavailability
in conscious rats. Pharmaceutical Research, 19, 1354–1361.
Horst, H. J., Holte, W. J., Dennis, M., Coert, A., Geelen, J., & Voigt, K.
D. (1976). Lymphatic absorption and metabolism of orally adminis-
tered testosterone undecanoate in man. Klinische Wochenschrift, 54,
875–879.
Humberstone, A. J., Porter, C. J. H., & Charman, W. N. (1996). A physi-
cochemical basis for the effect of food on the absolute bioavailability of
halofantrine. Journal of Pharmaceutical Sciences, 85, 525–529.
Ichihashi, T., Kinoshita, H., Shimamura, K., & Yamada, H. (1991). Ab-
sorption and disposition of epithiosteroids in rats (1): Route of admini-
stration and plasma levels of epitiostanol. Xenobiotica, 21, 865–872.
Ichihashi, T., Kinoshita, H., Takagishi, Y., & Yamada, H. (1991). Intrinsic
lymphatic partition rate of mepitiostane, epitiostanol and oleic acid
absorbed from rat intestine. Pharmaceutical Research, 8, 1302–1306.
Ichihashi, T., Kinoshita, H., Takagishi, Y., & Yamada, H. (1992a). Effect of
bile on absorption of mepitiostane by the lymphatic system in rats.
Journal of Pharmacy and Pharmacology, 44, 566–569.
Ichihashi, T., Kinoshita, H., Takagishi, Y., & Yamada, H. (1992b). Effect of
oily vehicles on absorption of mepitiostane by the lymphatic system in
rats. Journal of Pharmacy and Pharmacology, 44, 560–564.
Ichihashi, T., Kinoshita, H., & Yamada, H. (1991). Absorption and dispo-
sition of epithiosteroids in rats (2): Avoidance of first-pass metabolism
of mepitiostane by lymphatic absorption. Xenobiotica, 21, 873–880.
Johnson, J. M. (1976). Triglyceride biosynthesis in the intestinal mucosa. In
K. Rommel, H. Goebell, & R. Bohmer (Eds.), Lipid absorption: Bio-
chemical and clinical aspects ( pp. 85–94). Lancaster: MTP Press.
Kararli, T. T. (1995). Comparison of the gastrointestinal anatomy, physio-
logy, and biochemistry of humans and commonly used laboratory ani-
mals. Biopharmaceutics & Drug Disposition, 16, 351–380.
Levet-Trafit, B., Gruyer, M. S., Marjanovic, M., & Chou, R. C. (1996).
Estimation of oral drug absorption in man based on intestine perme-
ability in rats. Life Sciences, 58, PL359–PL363.
Liu, H.-X., Adachi, I., Horkoshi, I., & Ueno, M. (1995). Mechanism of
promotion of lymphatic drug absorption by milk fat globule membrane.
International Journal of Pharmaceutics, 118, 55–64.
Pahl, M. V., Oveisi, F., Khamiseh, G., & Vaziri, N. D. (1998). Intestinal
absorption and biliary secretion of cholesterol in rats with nephrotic
syndrome. Nephrology, Dialysis, Transplantation, 13, 1446–1451.
Palin, K. J., & Wilson, C. J. (1984). The effect of different oils on the
absorption of probucol in the rat. Journal of Pharmacy and Pharma-
cology, 36, 641–643.
Porter, C. J. H., Charman, S. A., & Charman, W. N. (1996). Lymphatic
transport of halofantrine in the triple-cannulated anaesthetized rat mo-
del: Effect of lipid vehicle dispersion. Journal of Pharmaceutical Sci-
ences, 85, 351–356.
Porter, C. J. H., & Charman, W. N. (1997). Uptake of drugs into the
intestinal lymphatics after oral administration. Advanced Drug Delivery
Reviews, 25, 71–89.
Porter, C. J. H., & Charman, W. N. (2001). Intestinal lymphatic drug trans-
port: An update. Advanced Drug Delivery Reviews, 50(1–2), 61–80.
Shah, N. H., Carvajal, M. T., Patel, C. I., Infeld, M. H., & Malick, A. W.
(1994). Self-emulsifying drug delivery systems (SEDDS) with polygly-
colyzed glycerides for improving in vitro dissolution and oral absorption
of lipophilic drugs. International Journal of Pharmaceutics, 106, 15–23.
Shiau, Y. -F. (1981). Mechanism of intestinal fat absorption. American
Journal of Physiology, 240, G1–G9.
Soria, I., & Zimmerman, C. L. (1996). The validation of the intestinal
permeability approach to predict oral fraction of dose absorbed in hu-
mans and rats. Biopharmaceutics & Drug Disposition, 17, 817–818.
Sugihara, J., & Furuuchi, S. (1988). Lymphatic absorption of hypolipidemic
compound 1-O-[p-(myristyloxy)-alpha-methylcinnamoyl]glycerol (LK-
903). Journal of Pharmacobio-Dynamics, 11, 121–130.
Sugihara, J., Furuuchi, S., Ando, H., Takashima, K., & Harigaya, S. (1988).
Studies on the intestinal lymphatic absorption of drugs: II. Glyceride
prodrugs for improving the lymphatic absorption of naproxen and nic-
otinic acid. Journal of Pharmacobio-Dynamics, 11, 555–562.
Thomson, A. B. R., Keelan, M., Garg, M. L., & Clandinin, M. T. (1989).
Intestinal aspects of lipid absorption: In review. Canadian Journal of
Physiology and Pharmacology, 67, 179–191.
Thomson, A. B., Schoeller, C., Keelan, M., Smith, L., & Clandinin, M. T.
(1993). Lipid absorption: Passing through the unstirred layers, brush
border membrane, and beyond. Canadian Journal of Physiology and
Pharmacology, 71, 531–555.
Tso, P. (1994). Intestinal lipid absorption. In L. R. Johnson (Ed.), Physio-
logy of the gastrointestinal tract (pp. 1867–1908). New York: Raven
Press.
Tucker, G. (1993). Drug Delivery: Lymphing along? Lancet, 341,
1314–1315.
Ueda, C. T., Lemaire, M., Gsell, G., & Nussbaumer, K. (1983). Intestinal
lymphatic absorption of cyclosporin A following oral administration in
an olive oil solution to rats. Biopharmaceutics & Drug Disposition, 4,
113–124.
Wasan, K. M. (2002). The role of lymphatic transport in enhancing oral
protein and peptide drug delivery. Drug Development and Industrial
Pharmacy, 28, 1047–1058.
Wasan, K.M., Ramaswamy, M., McIntosh, M.P., Porter, C.J., & Charman,
W.N. (1999). Differences in the lipoprotein distribution of halofantrine
are regulated by lipoprotein apolar lipid and protein concentration and
lipid transfer protein I activity: In vitro studies in normolipidemic and
dyslipidemic human plasmas. Journal of Pharmaceutical Sciences, 88,
185–190.
White, D. G., Story, M. J., & Barnwell, S. G. (1991). An experimental animal
model for studying the effects of a novel lymphatic drug delivery system
for propranolol. International Journal of Pharmaceutics, 69, 169–174.