A Case of Disseminated Cryptococcosis With Skin ... May-June Clinical Case.pdfSymptoms of...
Transcript of A Case of Disseminated Cryptococcosis With Skin ... May-June Clinical Case.pdfSymptoms of...

J La State Med Soc VOL 165 May/June 2013 171
CliniCal Case of the Month
A Case of Disseminated Cryptococcosis With Skin Manifestations in a Patient With Newly
Diagnosed HIV
Annette Zacharia; Muhammad F. Khan, MD; Anne E. Hull, MD; Appalanaidu Sasapu, MD; Michael A. Leroy, MD; Joanne T. Maffei, MD;
Akram Shakashiro, MD; Fred A. Lopez, MD
CASE REPORT
A 46-year-old man presented to the emergency depart-ment complaining of shortness of breath and a productive cough with white sputum and fever for one to two weeks. His symptoms did not resolve after being treated with short courses of outpatient oral antibiotics. The patient also ex-perienced intermittent headaches, an approximate weight loss of 15 pounds over four to six months, and a mildly pruritic rash on his face and upper body. He denied any associated neurologic symptoms, hemoptysis, chest pain, or night sweats. He had no recent sick contacts, no tuberculosis exposure, and no history of incarceration.
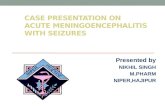
On physical exam, the patient was a thin appearing Caucasian man in mild distress. He had a temperature of 99 oF, heart rate of 102/minute, blood pressure of 103/66 mmHg, and respiratory rate of 36/min. His oxygen satura-tion was 97% on ambient room air and decreased to 95% with ambulation. Lung auscultation revealed decreased breath sounds in both lower lung zones but no evidence of crackles or wheezes. Physical examination was also signifi-cant for adherent white plaques with erythematous bases along the buccal mucosa and a diffuse macular rash, particu-larly on the extremities, with some associated excoriations. Umbilicated papules of the face and right shoulder that he attributed to bug bites were the most prominent feature of the rash (Figure 1). Additionally, he had an erythematous macular rash in a malar distribution and oily, flaky, white to yellowish scales on his face and chest. His conjunctivae were clear. There was no lymphadenopathy or hepato-splenomegaly and no appreciable focal neurological deficits.
The patient was found to be human immunodeficiency virus (HIV) antibody positive by ELISA that was confirmed by western blot. Advanced immunosuppression was confirmed with a CD4 count of 33 cells/mm3 (CD4 % of
4.3%) and an HIV viral load of 317,280 copies/ml. Chest radiograph revealed a focal egg-like calcification measuring approximately 2.4 cm in diameter in the left mid-lung zone overlying the left lateral posterior sixth and seventh ribs. His lactate dehydrogenase level was 245 µ/l (<201 µ/l), and arterial blood gas revealed an elevated alveolar-arterial gradient of 31 mmHg. He underwent a bronchoscopy on the second hospital day, and smear for Pneumocystis jiroveci pneumonia was positive. Several days into the hospital course, despite treatment for the pneumonia, he was still febrile, and his blood cultures were reported positive with encapsulated budding yeast confirmed as Cryptococcus neoformans.
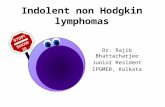
A non-contrast computed tomography scan of the head revealed no mass lesions or mass effect. A lumbar puncture was performed to evaluate for possible meningeal involvement. Opening pressure was 17 mm H2O. Analysis of cerebrospinal fluid (CSF) demonstrated a glucose level of 58 mg/dl, total protein of 47 mg/dl, and a cryptococcal antigen titer of 1:8. India ink stain of the CSF revealed encap-sulated yeast. CSF culture grew C. neoformans. Thereafter, the serum cryptococcal antigen titer was reported positive (>1:1024), in addition to confirmation of Cryptococcus in the respiratory sputum culture. The decision to perform a skin biopsy was made to demonstrate that the skin lesions were due to C. neoformans and not the umbilicated rash of molluscum contagiosum that it resembled. A skin biopsy confirmed the presence of Cryptococcus (Figure 2).
Laboratory analysis revealed a white blood cell count of 4.7 x 103/µl (4.5-10 x 103/µl), a hemoglobin of 14.4 gm/dl (13.0 -16.0 gm/dl), a hematocrit of 41.6% (39-46%), ferritin of 765.6 ng/ml (20-300 ng/ml), iron of 12 µg/dl (50-70 µg/dl), transferrin of 143 (200-360 mg/dl), total iron binding capacity of 186 µg/dl (250-425 µg/dl), and iron saturation of 6% (15-50%). Rapid plasma reagin and hepatitis serologies

172 J La State Med Soc VOL 165 May/June 2013
Journal of the Louisiana State Medical Society
were negative, and urinalysis showed no abnormalities. The patient’s serum was also negative for Toxoplasma IgG antibody and Histoplasma antigen. Ophthalmology exami-nation was notable for mild HIV retinopathy. The patient also had a negative tuberculosis interferon gamma release assay, and no acid fast organisms were present in the CSF.
DISCUSSION
Mycology, Ecology, & Epidemiology Each year, there are approximately 1 million new cases
of cryptococcosis and 625,000 deaths worldwide. The inci-dence of cryptococcosis has declined in developed countries after the introduction of antiretroviral therapy, but Cryp-tococcus is still among the leading causes of opportunistic infections in patients with acquired immune deficiency syndrome.1 There are two species that belong to the fungal genus Cryptococcus that infect humans, C. neoformans and C. gatti. C. gatti is associated with certain trees in nature and primarily infects healthy hosts. C. neoformans has been associated in soil samples inhabited especially by pigeons and can cause severe infections in individuals who are im-munosuppressed.2
PathogenesisAlthough cryptococcal infections can involve any
organ system, the organism has a predilection for the lung and central nervous system. Hosts acquire the infection via inhalation of the dessicated yeast cells or spores. Upon entering the lung, C. neoformans must face alveolar macro-phages, the host’s first line of defense. Various studies have shown that a major virulence factor of C. neoformans is its ability to avoid phagocytosis. Both antiphagocytic prop-
erties of the organism’s capsule itself and possible capsule-independent mechanisms through antiphagocytic proteins and signal-ing pathways are thought to contribute to its virulence.3 In healthy individuals, the C. neoformans cells are thought to be contained through a granulomatous response in the lungs, a response dependent on intact cellular immunity, causing only a mild or asymp-tomatic pulmonary infection. Hematogenous dissemination of the fungus to other organs is almost exclusively seen in immunocompro-mised individuals, usually occurring with CD4 counts <100 cells/µL, since they lack the ability to form a granulomatous reaction.3 A commonly infected anatomic site includes the central nervous system, resulting in menin-goencephalitis. Less commonly, dissemina-tion of the fungus can result in skin lesions.
CLINICAL PRESENTATION
Symptoms of meningoencephalitis may be indolent and typically include fever, mal-
aise, and headache; a skin rash can suggest a disseminated disease. Cutaneous manifestations occur in only 10-15% of patients with disseminated cryptococcal infection.4 Cutane-ous lesions can take on a variety of presentations including nodules, papules, pustules, ulcers, and may often mimic acne vulgaris, bacterial cellulitis, and cutaneous malignan-cies. The most commonly reported findings are those lesions similar to molluscum contagiosum.5 Molluscum contagio-sum, a large DNA poxvirus that causes a common, benign disease of childhood, can also infect adults. Molluscum con-tagiosum is spread by direct skin-to-skin contact or sexual transmission and can also occur in immunodeficient hosts. The characteristic presentation of molluscum contagiosum on the skin includes firm, dome-shaped papules with cen-tral umbilication. Molluscum contagiosum is self-limited in nature and often supportively treated. Although the diagnosis of molluscum contagiosum is frequently based on appearance of the skin lesions, opportunistic infections may often mimic molluscum contagiosum and can have serious consequences if not promptly treated. Thus, skin biopsy is useful for distinguishing molluscum contagiosum from other infections, such as cryptococcosis.6
LABORATORY DIAGNOSIS
Evaluation of patients with suspected cryptococcosis with cutaneous involvement is best accomplished through biopsy and culture results. C. neoformans is composed of a large polysaccharide capsule surrounding the cell wall. On biopsy, the cell wall will stain with either methenamine silver or periodic acid-Schiff, and the capsule will stain with mucicarmine or Alcian blue.7 In contrast, histologic
Figure 1: Centrally umbilicated, dome-shaped nodule on the right upper arm.

J La State Med Soc VOL 165 May/June 2013 173
examination of molluscum contagiosum typically reveals keratinocytes containing eosinophilic cytoplasmic inclu-sion bodies.8
Regardless of cutaneous involvement, a lumbar punc-ture is necessary for patients with neurologic symptoms or an underlying immunosuppressive illness in order to rule out meningoencephalitis. The opening pressure may be elevated (>200 mm H2O) on the initial lumbar puncture. India ink stain can be used to help identify C. neoformans in the CSF. The large polysaccharide capsule creates a halo-like appearance around the cell against a dark background cre-ated by the India ink. The CSF in HIV-infected individuals often has a lack of pleocytosis. Protein and glucose levels may be slightly abnormal. A normal CSF profile should not exclude the diagnosis of cryptococcus.9-10
While culturing remains the gold standard for estab-lishing a diagnosis of cryptococcal meningoencephalitis, it is cumbersome and time-intensive.10 Thus, testing for cryptococcal antigen in the CSF, detected with techniques such as latex agglutination, is important since it can con-firm the diagnosis and have prognostic indications. This test is very sensitive and is based upon the principle that anti-cryptococcal antibody-coated latex particles will ag-glutinate with antigens from the polysaccharide capsule.11 A CSF antigen titer >1:1024 is associated with a higher risk of mortality.10 Serum antigen testing is useful if patients cannot undergo lumbar punctures or if clinical suspicion remains high despite a negative India ink stain or normal CSF profiles.12
TREATMENT
The Infectious Disease Society of America practice guidelines state that treatment of cryptococcal dissemination, defined as involvement in at least two noncontiguous sites or evidence of high fungal burden on cryptococcal antigen titer, should be treated as if the patient has meningoencephalitis. Treatment for central nervous system-related cryptococcal infec-tion is divided into three phases: induction, consolidation, and maintenance. Induction therapy should last a total of 14 days and consist of intravenous amphotericin B (0.7-1.0 mg/kg per day) plus oral flucy-tosine (100 mg/kg per day) divided into four doses, followed by oral fluconazole (400 mg/day) for eight weeks during the consolidation phase. Since amphotericin is nephrotoxic, renal function must be moni-tored during treatment. In patients who are predisposed to renal dysfunction or are not tolerant of conventional amphotericin B, alternate lipid formulations are available.13 In addition, patients who show no clinical improvement after the two-week induction phase may warrant a repeat lumbar punc-
ture because the duration of the induction phase may need to be prolonged if persistent Cryptococcal neoformans cultures are present in the CSF. Monitoring of the serum cryptococ-cal antigen is not helpful since it does not correlate with clinical improvement.14 Thereafter, maintenance therapy consists of oral fluconazole (200 mg/day) for a minimum of 12 months, but there are no set guidelines in regards to duration of treatment as it depends on the immune status of the individual.13
SUMMARY
In this case report, we provide a concise review of the pathogenesis, clinical presentation, key diagnostic findings, and treatment options for Cryptococcus. Cryptococcus neofor-mans is a ubiquitous dimorphic fungus that can potentially be life threatening, especially in immunocompromised hosts. It commonly infects the respiratory tract or central nervous system. However, skin manifestations can be a marker of severe and disseminated disease, particularly in individuals at higher risk, including those patients with AIDS, cancer, long-term corticosteroid use, and organ trans-plant recipients. A timely diagnostic workup, including skin biopsy, blood cultures, and lumber puncture, is crucial since skin lesions may mimic other infectious processes. In addition, prompt, appropriate antifungal treatment should be initiated to decrease morbidity and mortality.
Figure 2: Biopsy of umbilicated papule on upper right arm. The fungal capsule of the organisms, as depicted by the arrow, stains with mucicarmine and may appear pink-to-red, confirming the diagnosis of Cryptococcus neoformans. (Mucicarmine stain, 40x magnification.)

174 J La State Med Soc VOL 165 May/June 2013
Journal of the Louisiana State Medical Society
REFERENCES
1. Park BJ, Wannemuehler KA, Marston BJ, et al. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS 2009; 23: 525–530.
2. Ellis DH, Pfeiffer TJ. Natural habitat of Cryptococcus neoformans var. gattii. J Clin Microbiol 1990; 28(7): 1642-1644.
3. García-Rodas, R, Zaragoza O. Catch me if you can: phagocytosis and killing avoidance by Cryptococcus neoformans. FEMS Immunol Med Microbiol 2012; 64(2): 147-161
4. Patel NC, Ewanowski C, Kupiec-Banasikowska A. Disseminated Cryptococcus neoformans: case report and review of the literature. Cutis 2009; 84(2):93-96.
5. Murakawa GJ, Kerschmann R, Berger T. Cutaneous Cryptococcus infection and AIDS. Report of 12 cases and review of the literature. Arch Dermatol 1996; 132(5):545-548.
6. Dohil MA, Lin P, Lee J, et al. The epidemiology of molluscum contagiosum in children. J Am Acad Dermatol 2006; 54(1): 47-54.
7. Schwartz J. The diagnosis of deep mycoses by morphologic methods. Hum Pathol 1982; 13(6): 519-533.
8. Cotell SL, Roholt NS. Images in clinical medicine. Molluscum contagiosum in a patient with the acquired immunodeficiency syndrome. N Engl J Med 1998; 338(13):888.
9. Graybill JR, Sobel J, Saag M, et al. Diagnosis and management of increased intracranial pressure in patients with AIDS and cryptococcal meningitis. The NIAID Mycoses Study Group and AIDS Cooperative Treatment Groups. Clin Infect Dis 2000; 30(1):47-54.
10. Rhein J, Boulware DR. Prognosis and management of cryptococcal meningitis in patients with human immunodeficiency virus infection. Neurobehavioral HIV Medicine 2012; 4:45-61
11. Heelan JS, Corpus L, Kessimian N. False-positive reactions in the latex agglutination test for Cryptococcus neoformans antigen. J Clin Microbiol 1991; 29(6): 1260-1261.
12. Chuck SL, Sande MA, Infections with Cryptococcus neoformans in the acquired immunodeficiency syndrome. N Engl J Med 1989; 321(12): 794-799.
13. Perfect JR, Dismukes WE, Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the infectious diseases society of america. Clin Infect Dis 2010; 50(3): 291-322.
14. Powderly WG, Cloud GA, Dismukes WE, et al. Measurement of cryptococcus antigen in serum and cerebrospinal fluid: value in the management of AIDS-associated cryptococcal meningitis. Clin Infect Dis 1994;18(5): 789-792.
Ms. Zacharia is a fourth-year Medical Student at Louisiana State University Health Sciences Center in New Orleans. Drs. Khan and Shakashiro are Fellows in the Department of Infectious Disease at LSUHSC-New Orleans. Dr. Hull is an Associate Professor of Clinical Medicine in the Department of Infectious Diseases at LSUHSC-New Orleans. Dr. Sasapu is currently undergoing a fellowship in Hematology/Oncology at the University of Arkansas for Medical Sciences. Dr. Leroy is a Resident in the Department of Pathology at LSUHSC-New Orleans. Dr. Maffei is an Associate Professor of Medicine in the Department of Infectious Diseases and Medical Director of MCL Infection Control Department at LSUHSC-New Orleans. Dr. Lopez is the Richard Vial Professor and Vice Chair for Education in the Department of Medicine at LSUHSC-New Orleans. He is also Section Editor for the Journal of the Louisiana State Medical Society.