3...Lalwani; Cur.pdf
-
Upload
pantas-saroha-siburian -
Category
Documents
-
view
217 -
download
0
Transcript of 3...Lalwani; Cur.pdf
-
8/14/2019 3...Lalwani; Cur.pdf
1/7
330 AJR:194, February 2010
tumors are characterized by KRAS mutations,-catenin and PTEN mutations are common-ly seen with endometrioid borderline ovar-ian tumors [4]. In addition, endometriosis isan important precursor of endometrioid andclear cell borderline ovarian tumors.
Serous borderline ovarian tumors areunique neoplasms that may behave in an ag-gressive fashion with associated peritonealimplants and regional lymphadenopathy.Because women with extraovarian spread ofdisease have a very good prognosis, the peri-toneal lesions are classied as implants in-stead of metastases. Although conservativemanagement sufces in women with early-stage borderline ovarian tumors wanting topreserve fertility, radical surgery is warrant-ed in patients with late-stage disease. In con-tradistinction to high-grade serous carcino-mas (the most common ovarian malignancy),borderline ovarian tumors are notoriously re-sistant to platinum-based chemotherapy [5].Prognosis is generally excellent. Althoughthe imaging features of borderline ovariantumors signicantly overlap with those of in-vasive epithelial cancers, cross-sectional im-
aging studies play a major role in the diagno-sis, management, and surveillance of patientswith borderline ovarian tumors [6].
Epidemiology and TaxonomyBorderline ovarian tumors are relative-
ly uncommon with an incidence of 1.52.5per 100,000 people per year. Approximately,3,000 cases of borderline ovarian tumors areannually diagnosed in the United States [7].Borderline ovarian tumors most commonly
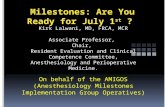
Current Update on BorderlineOvarian Neoplasms
Neeraj Lalwani 1Alampady K. P. Shanbhogue 1Raghunandan Vikram 2Arpit Nagar 3Jaishree Jagirdar 4Srinivasa R. Prasad 1
Lalwani N, Shanbhogue AKP, Vikram R, Nagar A,Jagirdar J, Prasad SR
1Department of Radiology, University of Texas HealthScience Center at San Antonio, 7703 Floyd Curl Dr.,San Antonio, TX 78 229. Address correspondence toS. R. Prasad ([email protected]).
2Department of Diagnostic Radiology, Division ofDiagnostic Imaging, University of Texas M.D. AndersonCancer Center, Houston, T X.
3Department of Radiology, Ohio State University MedicalCenter, Columbus, OH.
4Department of Surgical Pathology, University of TexasHealth Science Center at San Antonio, San Antonio, T X.
Wo m e ns I m ag i ng Rev i ew
AJR 2010; 194:330 336
0361803X/10/1942330
American Roentgen Ray Society
Borderline ovarian tumors com-prise up to 1520% of ovarian ep-ithelial neoplasms [1]. Borderlineovarian tumors a re histologically
characterized as epithelial tumors with a strat-ied growth pattern but without destructivestromal invasion. Serous and mucinous neo-plasms constitute the majority of borderlinetumors and occur mostly in women of repro-ductive age [1]. Howard C. Taylor, Jr., [2] iscredited with the rst use of the term semi-malignant tumors in 1929 for a subset oflarge ovarian tumors that had an indolent clin-ical course with relatively favorable patientoutcome despite the presence of peritonealdisease. However, borderline ovarian tumorswere not considered a distinct entity until 1971when the International Federation of Obstet-ric Gynecology (FIGO) established a separateborderline category of tumors. Since then,considerable controversy has surrounded thedenition and management of borderlineovarian tumors because of their enigmaticpathogenesis and perplexing biologic behav-ior [3]. Synonyms of borderline ovarian tu-mors include tumors of borderline malignan-
cy, tumors of low malignant potential, andatypical proliferative tumors.Several studies have described the char-
acteristic cytogenetics, epidemiology, natu-ral history, and biologic behavior of specicsubtypes of borderline ovarian tumors. Re-searchers have postulated that specic ge-netic changes contribute to their pathogenesisand stepwise progression to low-grade inva-sive ovarian carcinomas. Although the major-ity of serous and mucinous borderline ovarian
Keywords: borderline ovarian tumors, imagingneoplasms, ovarian cancer, ovarian tumors of lowmalignant potential
DOI:10.2214/AJR.09.3936
Received November 9, 2009; accepted after revisionNovember 13, 2009 .
W O M E N S
I M A G I N G F O C U S O N :
OBJECTIVE. Borderline ovarian tumors comprise a unique group of noninvasive ovarianneoplasms with characteristic histology and variable tumor biology that typically manifest aslow-stage disease in younger women with resultant excellent prognosis.
CONCLUSION. Borderline tumors are considered to be precursors of low-grade ovar-ian cancers. Accurate diagnosis and staging facilitate optimal patient management particu-larly in patients desiring to preserve fertility.
Lalwani et al.Borderline Ovarian Neoplasms
Womens ImagingReview
-
8/14/2019 3...Lalwani; Cur.pdf
2/7
AJR:194, February 2010 331
Borderline Ovarian Neoplasms
affect white women of reproductive age typi-cally during the fourth decade. Up to 27% ofpatients with borderline ovarian tumors areyounger than 40 years [8]. The mean age ofpresentation of borderline ovarian tumors isapproximately 20 years earlier than that of in-vasive ovarian carcinomas [9]. Most patientswith borderline tumors present with nonspe-cic symptoms such as abdominopelvic painor mass. Approximately 16% of patients areasymptomatic at the time of diagnosis [10].According to the 2003 World Health Orga-nization classication schemata [11], border-line ovarian tumors are classied on the ba-sis of histopathology and histogenesis intoserous, mucinous, endometrioid, clear cell , and transitional (Brenner) subtypes. Salientfeatures, including precursor lesions and cy-togenetics, of borderline ovarian tumors aresummarized in Table 1.
Serous Borderline Ovarian TumorsSerous borderline ovarian tumors com-
prise the most common histologic subtypeof borderline ovarian tumors, accounting forapproximately 65% of all borderline ovari-an tumors [12]. The mean age range of pre-sentation is 3440 years. Serous borderlineovarian tumors are slow-growing neoplasmsthat may be associated with aggressive bio-logic behavior in the form of peritoneal im-plants and regional lymphadenopathy inapproximately 35% and 27% of patients, re-spectively. Histologically, serous borderlineovarian tumors are divided into typical, 90%of serous borderline ovarian tumors, and mi-cropapillary, 10% of serous borderline ovari-an tumors, types [11]. Most low-grade serouscarcinomas are thought to arise from micro-papillary borderline ovarian tumors. Seroussurface borderline tumor is another variant
that shows polypoid excrescences that occu-py the outer surface of the ovary.
Recent advances in cytogenetics haveyielded unique insights into the pathogen-esis and biologic behavior of serous border-line ovarian tumors. In several studies, inves-tigators have found that only a small subset ofserous cystadenomas progress to serous bor-derline ovarian tumors and that activatingmutations of BRAF and KRAS genes are ear-ly events in tumorigenesis of borderline ovar-ian tumors. In contradistinction to high-gradeserous carcinomas, the most common sub-type of ovarian cancer, that are characterizedby p53 mutations in more than 50% tumors,serous borderline ovarian tumors are charac-terized by KRAS and BRAF mutations in twothirds of tumors (Fig. 1). Up to 50% of serousborderline ovarian tumors are characterizedby BRAF mutations, and KRAS mutations are
TABLE 1: Summary of Borderline Ovarian Tumors
Type of BorderlineOvarian Tumor Precursor Progression to Cytogenetics Characteristic Features Prognosis
Serous Serous cystadenoma oradenobroma
Invasive low-gradeserous carcinoma
Mutations in KRAS orBRAF genes 67%
May follow dualistic oncogenicpathway; invasive or noninvasiveimplants may occur; presence ofinvasive implants is a poorprognostic factor; associatedwith regional lymphadenopathy
Typical subtype (90%)
Micropapillary subtype (10%) isclosely associated with invasiveimplants
70% of cases are stage I;survival is almost 100%
30% of cases are advancedstages; survival is 95.3% ifimplants are noninvasiveand 66% if implants areinvasive
Mucinous Intestinal subt ype (9 0%):mucinous cystadenoma
Mllerian subtype (10%):endometriotic cysts?
Intraepithelialcarcinoma then toinvasive mucinouscarcinoma
Mutations in KRAS (> 60%) Intestinal subtype (90%) isunilateral; is multicystic withsmooth capsule; is associatedwith pseudomyxoma peritonei;has larger multilocular cysticlesions; shows uids of differentsignal intensities on T1- orT2-weighted MR images
Mllerian subtype (10%) isbilateral in 2030%; is exophyticand paucilocular; mimics serous tumors hence termed seromuci-nous; implants may present
82% of cases are stage I;5-year survival is up to99100%
18% of cases are advancedstages; mortality mayreach up to 50% dependingon stage
Endometrioid Endometriosis, endo-
metrioid adenobroma
Intraepithelial
carcinoma then tolow-grade invasiveendometrioidcarcinoma
Gene mutations in
-catenin (> 50%); loss ofheterozygosity or PTEN mutations (20%);microsatellite instability(1350%)
None Benign course with high
survival rates
Clear cell Endometriosis, clear celladenobroma
Intraepithelialcarcinoma then toinvasive clear cellcarcinoma
KRAS mutations (516%);microsatellite instability( 13%)
None Benign course with highsurvival rates
Brenner Benign Brenner Malignant Brenner? Not yet identied None Benign course with highsurvival rates
-
8/14/2019 3...Lalwani; Cur.pdf
3/7
332 AJR:194, February 2010
Lalwani et al.
seen in more than a third of serous borderlineovarian tumors.
A dual oncogenic pathway has been de-scribed in which serous borderline ovariantumors undergo stepwise transformation tolow-grade serous carcinomas and high-gradeserous carcinomas possibly arise de novofrom surface epithelia due to p53 and BRCA mutations [1315]. Serous borderline ovari-an tumors are characterized by activation ofspecic tumor suppressor genes ( SERPINA5 and dual specicity phosphatase 4 [ DUSP4 ])that inhibit degradation of the extracellu-lar matrix, a key event in the pathogenesisof invasive growth [16]. Thus, serous bor-derline ovarian tumors charter an indolentcourse due to genetic events that promote tu-mor proliferation but not metastases. In addi-tion, pharmacologic inhibitors of the KRAS
BRAF pathway are being considered to treatpatients with advanced serous borderlineovarian tumors to improve patient survival.
The serous borderline ovarian tumors areunique among the borderline ovarian tumorsin that invasive or noninvasive peritoneal im-plants may occur in 35% of cases. The no-menclature is dependent on whether theimplants are simply stuck on the perito-neal surfaces (noninvasive) or have invadedthe underlying tissue such as omentum andbowel wall [3]. Although noninvasive im-plants are associated with benign behavior,the presence of invasive implants portendsa poor prognosis [11, 17]. A small subset of
implants also may originate de novo fromnodal endosalpingiosis (spectrum of second-ary mllerian system involvement in the pel-vis) [3]. Psammoma bodies may be associ-ated with noninvasive implants.
Lymph node involvement may be seen inabout 27% of serous borderline ovarian tu-mors [18]. Although lymph node involvementhas no prognostic value, lymph nodes mayserve as sites of recurrence and progressionto carcinoma [18, 19]. It is hypothesized thatthese nodal metastases most likely exit theovary through the peritoneal lymphatics rath-er than through the ovarian lymphatics. Com-monly involved lymph nodes in advanced se-rous borderline ovarian tumors include thefollowing in descending order of frequency:pelvic, omental and mesenteric, and paraaor-tic and supradiaphragmatic regions [19].
Serous borderline ovarian tumors manifestas complex cystic adnexal masses with thinseptations and endocystic or exocystic veg-etations [20] (Fig. 2). The solid componentscommonly show moderate enhancement dur-
ing contrast-enhanced CT or dynamic MRI(Fig. 3). Approximately one third of serousborderline ovarian tumors are bilateral. Non-invasive peritoneal implants occur more fre-quently than invasive implants (78% vs 22%,respectively) [12]. A serous tumor with in-vasive implants macroscopically may haveprofuse papillary projections that actual-ly consists of many vesicles perforating andextending beyond the ovarian capsule with-out a solid component. The lesion may havehigh signal intensity on contrast-enhanced T1-weighted imaging and water signal intensityon the T2-weighted imaging, suggesting the
absence of solid elements [21]. Barring thepresence of extraovarian disease (Fig. 4), theimaging ndings of serous borderline ovariantumors are indistinguishable from other bor-derline ovarian tumors and advanced border-line ovarian tumors masquerade as invasiveovarian carcinomas.
At the time of presentation, 70% of serousborderline ovarian tumors a re conned to theovary (stage I). Survival for women with stageI tumors is vir tually 100%. The overall prog-nosis is dependent on the presence of perito-neal implants. After 7.4 years (mean) of fol-low-up, the survival for advanced stage serous
Fig. 352-year-old woman
with serous carcinomawith background serousborderline tumor. Axialcontrast-enhanced CTscan through pelvis showsleft ovarian cystic lesion(arrowheads ) with multipleenhancing intracystic solidpapillary excrescences.Surgical excision conrmeddiagnosis of serouscarcinoma with backgroundserous borderline tumor.
Serous cystadenoma
Serous borderline tumor
Low-grade serous carcinoma
Mutations in BRAF or KRAS
Fig. 1Schematic representation shows progressionof serous borderline tumor to low-grade serouscarcinoma.
AFig. 2Benign serous cystadenoma versus serous borderline tumor: imaging ndings.A, 46-year-old woman with benign serous cystadenoma. Axial T2-weighted MR image shows well-denedhyperintense cystic lesion ( arrowheads ) in pelvis without mural nodules or solid components. Surgical excisionconrmed diagnosis of left ovarian serous cystadenoma.B, 45-year-old woman with serous borderline tumor. Axial contrast-enhanced CT image through pelvis showswell-dened cystic lesion with thin internal septations ( arrowhead ) and eccentric wall thickening along rightanterolateral wall ( arrow ).
B
-
8/14/2019 3...Lalwani; Cur.pdf
4/7
AJR:194, February 2010 333
Borderline Ovarian Neoplasms
stage in the orderly, stepwise progression toinvasive carcinoma akin to the adenomacar-cinoma sequence in colorectal carcinomas.Mucinous borderline ovarian tumors are as-sociated with KRAS mutations in more than60% of cases. The increasing frequency ofKRAS mutations (3386%) has been de-scribed in mucinous cystadenomas, border-line ovarian tumors, and carcinomas [4, 13].
On imaging, mucinous borderline ovariantumors may be twice the size of serous bor-derline ovarian tumors and may manifest asmultilocular or unilocular cystic masses (Figs.5 and 6). Mucinous borderline ovarian tu-mors commonly appear as multilocular cys-tic masses with numerous septa and containuids of different signal intensities on T1- orT2-weighted MR images [20]. The endocysticvegetations of mucinous borderline ovarian tu-
mors show delayed uptake of contrast medium.On T1-weighted images, the mucinous compo-nent may impart a high signal intensity.
The imaging features of mllerian muci-nous borderline ovarian tumors arising fromendometriotic cysts are distinctive. The ml-
borderline ovarian tumors with noninvasiveimplants is 95.3%, whereas survival for pa-tients with tumors with invasive implants is66% [19]. Micropapillary architecture in theprimary ovarian tumor is closely associatedwith the presence of invasive implants [10].Serous borderline ovarian tumors with inva-sive and noninvasive implants may have 45%and 11% recurrence rates, respectively, over aperiod of 15 years [20]. The tumors usuallyrecur as invasive carcinomas in up to 77% ofpatients, with a high rate of resultant mortal ity(up to 74%) [22].
Mucinous Borderline Ovarian TumorsMucinous borderline ovarian tumors com-
prise about 32% of all borderline ovarian tu-mors [12]. The mean age of presentation is 45years. Mucinous borderline ovarian tumors
consist of two distinct histologic subtypes: theintestinal (90%) and the mllerian (endocer-vicallike, 10%) histotypes [11]. The intestinalsubtype is usually unilateral and may coexistwith pseudomyxoma peritonei in up to 17% ofcases [1]. The mllerian subtype is bilateral in
up to 40% cases and coexists with ipsilateralovarian or pelvic endometriosis in 2030% ofcases [1, 11]. The mllerian mucinous border-line ovarian tumors mimic serous borderlineovarian tumors to an extent and hence are alsotermed seromucinous borderline ovarian tu-mors. Like serous borderline ovarian tumors,these tumors may be associated with abdomi-nal or pelvic implants, which may be invasivein some cases.
Before the diagnosis of mucinous border-line ovarian tumor is made, it is important toexclude a metastatic adenocarcinoma, mostcommonly from the gastrointestinal tract,usually an appendiceal or colonic primary.Immunohistochemistry using a cytokeratinpanel is useful in differentiating metastaticversus primary ovarian tumors [3].
There is strong evidence that the muci nous
borderline ovarian tumors associated withpseudomyxoma peritonei (i.e., ascites withabundant mucoid or gelatinous material) areactually metastatic rather than an ovarian pri-mary [3, 11]. Mucinous borderline ovarian tu-mors are thought to represent an intermediate
A
Fig. 4Serous implants.A, 48-year-old woman with noninvasive implantsshowing psammomatous calcications. Axial CTimage through pelvis shows midline paraumbilicalcalcied implant ( arrow ) in anterior abdominal wall.B, 37-year-old woman with right paracolic invasiveimplants (arrow ).
B
A
Fig. 544-year-old woman with mucinous borderline tumor.A and B, Transvaginal ultrasound images show large multiloculated cystic mass with thick internal septations and small solid components ( arrowhead , B). Largerloculation (star , A) on left anterolateral aspect shows ne internal echoes.C, Axial contrast-enhanced CT image through pelvis shows large cystic mass ( arrowhead ) with thick septations and mural nodules along periphery.
CB
-
8/14/2019 3...Lalwani; Cur.pdf
5/7
334 AJR:194, February 2010
Lalwani et al.
lerian mucinous borderline ovarian tumorsare typically uni- or paucilocular cystic mass-es with mural nodules (Figs. 7 and 8). The u-id component shows high intensity on bothT1- and T2-weighted images. The mural nod-ule shows high intensity on T2-weighted im-ages as well as contrast enhancement [23].
At the time of diagnosis, approximately82% mucinous borderline ovarian tumorsare conned to the ovary and clinically be-have similarly to serous borderline ovariantumors with 5-year survival rates of up to99100% [24]. Patients with these tumorsrarely have a recurrence or die of the disease.
Advanced-stage (18%) mucinous borderlineovarian tumors, however, may have a mortal-ity up to 50% that is stage dependent [13].
Miscellaneous Borderline TumorsUncommon subtypes of borderline ovar-
ian tumors encompass 34% all borderlineovarian tumors and include endometrioid,clear cell, and transitional cell (Brenner va-riety) tumors. Endometrioid borderline ovar-ian tumors resemble analogous endometrioidtumors arising from the uterine corpus andarise either from the surface ovarian epitheli-um or from endometriosis. Clear cell border-line ovarian tumors are ovarian tumors of lowmalignant potential characterized by the pres-ence of clear or hobnail cells set in a densebrous stroma with absence of stromal inva-sion. Borderline Brenner tumors are ovariantransitional cell tumors with atypical or ma-lignant features of the epithelium but lackingstromal invasion. The mean age for miscella-neous borderline ovarian tumors ranges be-tween 45 and 65 years.
Endometriosis and endometrioid adeno-bromas serve as precursors of endometri-oid borderline ovarian tumors. In contrast toserous and mucinous borderline ovarian tu-mors, endometrioid borderline ovarian tu-mors are characterized by mutations involv-ing the -catenin gene (50%), PTEN gene(20%), and microsatellite instability (up to50%) [11]. Endometrioid borderline ovariantumors have the potential to progress to low-grade invasive carcinoma. Although clear cellborderline ovarian tumors have been associ-ated with endometriosis and adenobromas, a
stepwise molecular pathway for the progres-sion of endometriosis or adenobroma to clearcarcinoma has not yet been elucidated. Clearcell borderline ovarian tumors are character-ized by KRAS mutations (516%) and micro-satellite instability (13%) [15]. Molecular andgenetic changes in Brenner tumors have notyet been described [4, 13].
Nonserous, nonmucinous borderline ovar-ian tumors do not show characteristic imag-ing features and may resemble other border-line ovarian tumors as well as early-stageovarian carcinomas (Fig. 9). The miscella-
Fig. 7Mllerian borderline tumors.A, 46-year-old woman with mllerian borderline tumor. Axial fat-suppressed T2-weighted image through pelvisshows unilocular cystic lesion with small eccentric hyperintense mural nodule ( arrow ).B, 52-year-old woman with mucinous (mllerian subtype) borderline tumor with background endometrioticcyst. Axial CT image through pelvis shows small unilocular lesion with enhancing mural nodules ( arrow ).
Fig. 648- year-old woman with unilocularmucinous borderline tumor. Sagittal T2-weightedMR image through pelvis shows large unilocularcystic mass ( arrowheads ) without internalseptations or mural nodules.
BA
Fig. 849-year-old woman with mucinousadenocarcinoma in background of mucinousborderline tumor. Axial contrast-enhanced CT image through pelvis shows large multiloculated cysticlesion with irregular and thick internal septations(white arrow ). There is noticeable variation indensities of various loculi; some loculi ( stars ) appearhyperdense in comparison with others. Intracysticenhancing mural nodules and solid components(black arrows ) are visualized along left anterior wall.
Fig. 941-year-old woman with endometrioidborderline ovarian tumor. Axial contrast-enhancedCT image through pelvis shows unilocular cysticlesion with mural nodule along left posterolateral wall(arrowhead ) mimicking low-grade carcinoma.
-
8/14/2019 3...Lalwani; Cur.pdf
6/7
AJR:194, February 2010 335
Borderline Ovarian Neoplasms
neous borderline ovarian tumors chart a be-nign course after tumor removal with excep-tionally rare recurrences or metastasis. Thesurvival rate is up to 100%.
Imaging Algorithm for the Diagnosisof Borderline Ovarian Tumors
Borderline ovarian tumors commonlypresent as adnexal masses. Accurate diag-nosis and distinction from advanced ovarianmalignancy facilitate management includingfertility-preserving surgery. Transvaginalsonography is the primary screening imag-ing technique in the evaluation of any sus-pected adnexal mass [25, 26]. Borderlineovarian tumors manifest usually as complexcystic masses with septations and occasion-ally as mural nodules.
The use of color and spectral Doppler ul-trasound may provide additional informationabout tumoral angioarchitecture. However,gray-scale and color Doppler sonograms havebeen shown to be of limited value in charac-terizing borderline ovarian tumors. Adnex-al lesions may, at best, be categorized as be-nign or aggressive on sonography. MRI andMDCT can characterize adnexal masses intobenign and malignant in up to 93% [27, 28]and 89% [29] of the cases, respectively. Sono-graphically indeterminate lesions thus requireMRI for fur ther characterization (Fig. 10).
MRI, on account of its superior soft-tissuedistinction and multiplanar capabilities, al-lows better characterization of complex cystic
masses particularly with regard to the depic-tion of septations and mural nodules. Dynam-ic MRI characteristics of ovarian tumors haverecently been studied [3032], rst during thearterial phase (30-second delay) and on de-layed contrast-enhanced MR images (> 4 min-utes). The timeintensity curves of borderlineovarian tumors were compared with those ofnormal outer myometrium. Although the tu-mors that showed a gradual increase in en-hancement without a well-dened peak werecorrelated to benign ovarian tumors, border-line ovarian tumors showed moderate initialenhancement followed by a plateau.
Both MRI and MDCT can be used to mapperitoneal disease and provide informationfor preoperative planning and staging. Bor-derline ovarian tumors are not PET-avid andhence are interpreted as benign tumorson FDG PET [33, 34]. Ovarian masses thatshow complex features on MRI that are con-cerning for malignancy but appear as be-nign on PET are said to be characteristic ofborderline ovarian tumors [33]. However, -
nal diagnosis and staging of borderline ovar-ian tumors require pathologic evaluation af-ter surgical excision [5].
Staging, Management, andSurveillance Algorithm
Borderline ovarian tumors follow a stag-ing system similar to that used for stagingovarian epithelial carcinomas. The staging issurgical and the suggested guidelines includetaking specimens from the omentum; intesti-nal serosa and mesentery; pelvic peritoneumincluding the cul-de-sac, bladder peritone-um, and pelvic wall; and abdominal perito-neum including paracolic gutters, diaphrag-matic surface, and retroperitoneal nodes [1,
5]. The FIGO staging for borderline ovariantumors is summarized in Table 2.
When postoperative surgical staging as-certains borderline ovarian tumors withoutinvasion, peritoneal seeding, or distant me-tastasis, no further treatment is required.However, advanced-stage disease requirescytoreduction surgery with or without plat-inum-based chemotherapy. Patients with asuspected borderline ovarian tumor and de-siring fertility preservation may opt for aconservative approach such as cystectomyor salpingo-oophorectomy instead of radi-cal surgery. An outline of optimized patientmanagement is depicted in Figure 11.
Follow-up is usually a combination of clin-ical examination, transvaginal ultrasound,and CA-125 levels. During the initial 2 years,
follow-up evaluation is performed every 3months. Patients are then evaluated biannual-
Adnexal lesion
Transvaginal ultrasound
Staging (borderline tumors may be diagnosed as benign on MRI)
Conservative surger y Radical surgery
Benign Non-benign
Benign or borderlineovarian tumor
Malignant
MRI
Fig. 10Imaging algorithmfor diagnosis of borderline tumors.
No invasive implants
Borderline ovarian tumors
Surgical staging
Follow-up
Salpingo-oophorectomy Cystectomy
Invasive implants present
Both ovaries involvedor one ovary present
One ovary involved
Want fertility conservationRadical surgery
Transvaginal ultrasound, clinical examination, and CA-125 levels
Fig. 11Schematicrepresentation ofmanagement andsurveillance algorithmfor borderline ovarianneoplasms. Information from[5] was incorporated in thisalgorithm.
-
8/14/2019 3...Lalwani; Cur.pdf
7/7
336 AJR:194, February 2010
Lalwani et al.
ly for 35 years after surgery and then annual-ly thereafter [5]. Transvaginal sonography orpelvic MRI may be performed for the detec-tion of local recurrence. MDCT is better suit-ed for the detection of peritoneal disease orextrapelvic spread of disease.
ConclusionBorderline ovarian tumors are an interest-
ing subset of epithelial neoplasms that affectyounger women in the reproductive age group,chart an indolent course, and show excellentprognosis. Borderline tumors typically mani-fest as complex cystic masses with mural nod-ularity and septations. The imaging ndingsmay be indistinguishable from those of inva-sive ovarian carcinomas. Fertility-sparing sur-gery may sufce in patients with tumors thatare conned to the ovary. Radical surgery isrecommended in patients with advanced dis-ease. Long-term surveillance is recommendedto document and treat late recurrences.
References
1. Acs G. Serous and mucinous borderline (low ma-lignant potential) tumors of the ovary. Am J Clin
Pathol 2005; 123[suppl]:S13S57
2. Taylor HC Jr. Malignant and semi malignant tumours
of the ovary. Surg Gynecol 1929; 48:204230
3. Silverberg S. Borderline ovarian tumors: consen-
sus, controversy, and continuing challenges.
Pathol Case Rev 2006 ; 11:917
4. Bast RC Jr, Hennessy B, Mills GB. The biology of
ovarian cancer: new opportunities for translation.
Nat Rev Cancer 2009; 9:415428
5. Cadron I, Leunen K, Van Gorp T, Amant F, Neven
P, Vergote I. Management of borderline ovarian
neoplasms. J Clin Oncol 2007; 25:29282937
6. deSouza NM, ONeill R, McIndoe GA, Dina R,Soutter WP. Borderline tumors of the ovary: CT and
MRI features and tumor markers in differentiation
from stage I disease. AJR 2005; 184:9991003
7. Gershenson DM. Clinical management potential
tumours of low malignancy. Best Pract Res Clin
Obstet Gynaecol 2002; 16:513527
8. Swanton A, Bankhead CR, Kehoe S. Pregnancy
rates after conservative treatment for borderline
ovarian tumours: a systematic review. Eur J Ob-
stet Gynecol Reprod Biol 2007; 135:37
9. Gotlieb WH, Chetrit A, Menczer J, et al. Demo-
graphic and genetic characteristics of patients
with borderline ovarian tumors as compared to
early stage invasive ovarian cancer. Gynecol On-
col 2005; 97:780783
10. Webb PM, Purdie DM, Grover S, Jordan S, Dick
ML, Green AC. Symptoms and diagnosis of bor-
derline, early and advanced epithelial ovarian
cancer. Gynecol Oncol 2004; 92:232239
11. Tavassoli FA, Devilee P. World Health Organiza-
tion classication of tumors: pathology and ge-
netics of tumors of the breast and female genital
organs . Lyon, France: IARC Press, 2003
12. Jones MB. Borderline ovarian tumors: current
concepts for prognostic factors and clinical man-
agement. Clin Obstet Gynecol 200 6; 49:517525
13. Kurman RJ, Shih IeM. Pathogenesis of ovarian
cancer: lessons from morphology and molecular
biology and their clinical implications. Int J Gy-
necol Pathol 2008; 27:151160
14. Shih IeM, Kurman RJ. Ovarian tumorigenesis: a
proposed model based on morphological and mo-
lecular genetic analysis. Am J Pathol 2004;164:15111518
15. Shih IeM, Ku rman RJ. Molecula r pathogenesis of
ovarian borderline tumors: new insights and old
challenges. Clin Cancer Res 20 05; 11:72737279
16. Sieben NL, Oosting J, Flanagan AM, et al. Dif-
ferential gene expression in ovarian tumors re-
veals Dusp 4 and Serpina 5 as key regulators for
benign behavior of serous borderline tumors. J
Clin Oncol 2005; 23:72577264
17. Bell DA, Scully RE. Ovarian serous borderline
tumors with stromal microinvasion: a report of 21
cases. Hum Pathol 1990; 21:397403
18. Fadare O. Recent developments on the sign i-
cance and pathogenesis of lymph node involve-ment in ovarian serous tumors of low malignant
potential (borderline tumors). Int J Gynecol Can-
cer 2009 ; 19:103108
19. Seidman JD, Kurman RJ. Ovarian serous border-
line tumors: a critical review of the literature with
emphasis on prognostic indicators. Hum Pathol
2000 ; 31:539557
20. Bent CL, Sahdev A, Rocka ll AG, Singh N, Sohaib
SA, Reznek RH. MRI appearances of borderline
ovarian tumours. Clin Radiol 2009; 64:430438
21. Ohta T, Ohmichi M, Hayasaka T, et al. Character-
istic features of ovarian borderline tumors with
invasive implant. Arch Gynecol Obstet 2005;
272:278282
22. Wu TI, Lee CL, Wu MY, et al. Prognostic factors
predicting recurrence in borderline ovarian tu-mors. Gynecol Oncol 200 9; 114:237241
23. Kataoka M, Togashi K, Koyama T, et a l. MR im-
aging of mllerian mucinous borderline tumors
arising from endometriotic cysts. J Comput Assist
Tomogr 2002; 26:532537
24. Prat J. Pathology of the ovary. Philadelphia, PA:
Saunders, 2004
25. Lin PS, Gershenson DM, Bevers MW, Lucas KR,
Burke TW, Silva EG. The current status of surgi-
cal staging of ovarian serous borderline tumors.
Cancer 1999; 85:905911
26. Zanetta G, Rota S, Lissoni A, Meni A, Brancatelli
G, Buda A. Ultrasound, physical examination, and
CA 125 measurement for the detection of recur-
rence after conservative surgery for early borderline
ovarian tumors. Gynecol Oncol 2001; 81:6366
27. Hricak H, Chen M, Coakley FV, et al. Complex
adnexal masses: detection and characterization
with MR imaging: multivariate analysis. Radiol-
ogy 2000; 214:3946
28. Sohaib SA, Sahdev A, Van Trappen P, Jacobs IJ,
Reznek RH. Characterization of adnexal mass le-
sions on MR imaging. AJR 2003; 180:12971304
29. Tsili AC, Tsampoulas C, Charisiad i A, et al. Adn-
exal masses: accuracy of detection and differen-
tiation with multidetector computed tomography.
Gynecol Oncol 2008; 110:223130. Bazot M, Nassar-Slaba J, Thomassin-Naggara I,
Cortez A, Uzan S, Darai E. MR imaging compared
with intraoperative frozen-section examination for
the diagnosis of adnexal tumors: correlation with
nal histology. Eur Radiol 2006; 16:26872699
31. Thomassin-Naggara I, Bazot M, Darai E, Callard
P, Thomassin J, Cuenod CA. Epithelial ovarian
tumors: value of dynamic contrast-enhanced MR
imaging and correlation with tumor angiogenesis.
Radiology 2008; 248:148159
32. Thomassin-Naggara I, Cuenod CA, Darai E, Mar-
sault C, Bazot M. Dynamic contrast-enhanced
MR imaging of ovarian neoplasms: current status
and future perspectives. Magn Reson ImagingClin N Am 2008; 16:661672
33. Risum S, Hogdall C, Loft A, et al. The diagnostic
value of PET/CT for primary ovarian cancer: a pro-
spective study. Gynecol Oncol 2007; 105:145149
34. Jung DC, Choi HJ, Ju W, Kim SC, Choi KG. Dis-
cordant MRI/FDG-PET imaging for the diagno-
sis of borderline ovarian tumors. Int J Gynecol
Cancer 2008; 18:637641
TABLE 2: Summary of International Federation of Obstetric Gynecology(FIGO) Staging
FIGO Stage Denition
I Tumor conned to ovary
II Peritoneal implants within the pelvis
III Peritoneal implants beyond the pelvis, posit ive lymph nodes, or both
IV Liver parenchyma involvement or tumor beyond the peritoneal cavity