3.2. Medicine_Acute Coronary Syndromes 2014A
Transcript of 3.2. Medicine_Acute Coronary Syndromes 2014A
-
7/27/2019 3.2. Medicine_Acute Coronary Syndromes 2014A
1/4
JMA-1, JMA-2, Telma | Claveria Page 1 of4
November 12, 2012
Acute Coronary SyndromesDr. Uy
OUTLINE
I. Acute Coronary Syndromesa. Clinical Datab. Signsc. Initial Investigationd. Subsequent Investigatione. ECG Changesf. Biomarkersg. Assessment and Treatment of ACS
II. Complications of MIIII. Coronary Artery DiseaseIV. Unstable Angina/ NSTEMI
ACUTE CORONARY SYNDROMES
Represent a dynamic spectrum of similar disease process, beingpart of a continuum of ischemic coronary disease
Each syndrome is associated with specific strategies in prognosisand management
Figure 1. Spectrum of Acute Coronary Syndromes
Composed of patients with Acute Myocardial Infarction with ST-segment Elevation (STEMI), Non-ST-segment Elevation MI
(NSTEMI) and Unstable Angina,All present with chest pain
Biomarkers for MI- Troponin T, Troponin I, CPK
Figure 2. Sequelae of Coronary Thrombus
Figure 3. Thrombus formation and ACS.
Starts with thrombus formation then becomes either:o Unstable Angina: plaque with a small fissure sudden formation of
small clot (dark red) cause sudden decrease of blood flow sudden
ischemic episode unstable angina
o NQMI (Non-Q-wave MI): there is increased myocardial necrosis but noQ wave incomplete (note: both UA and NQMI are called Non-STEM
ACS)
o STEMI: at bigger area complete obstructiono ACI (acute coronary insufficiency): prolonged chest pain > 20mins, with
(+) ST changes and enzyme/ biomarker elevationo ST-elevation MI (STEMI): prolonged chest paon (>20 mins), persisting ST
elevation despite NTG. The ST elevation is at least 1mm in 2 adjacen
leads, or at least 2 mm in 2 adjacent precordial leads.
oLeft Bundle Branch Block (recent)
Figure 4. Course of Myocardial Hypoxia
CLINICAL DATA Chest paino Typical chest pain, severe but prolonged and sense of impending death
(Angor Animi)
o Nausea, vomiting, sweating, dizziness, extreme weakness and dyspnea Symptoms of complications o Dyspnea, PND, irritability, palpitation
Silent painless myocardial infarction (but with other symptoms likedyspnea, paroxysmal nocturnal dyspnea irritability or palpitation)
Common in diabetics and stroke patients because sensation andperception maybe altered and they cannot complain of pain.
SIGNS Anxious patient Signs of cardiogenic shock if present Cold sweats Peripheral cyanosis Hypotension, thready pulse Oliguria Pulse: Arrhythmias may be detected Low grade fever due to necrosis & inflammation Auscultation:o First heart sound (S1) is weak because contractility is impairedo Pulmonary components of S2 may be accentuated resulting to
pulmonary HTN
o Third heart sound (S3 gallop)o Pericardial frictioin rub if pericarditis occurso Murmur of mitral regurgitation or VSD if complications occuro Moist rales may be heard at the base of the lungs
Note: In some cases, auscultation may reveal no abnormality
INITIAL INVESTIGATIONS Immediate ECGo ECG is sole test required to select patients for emergency reperfusion
(thrombolysis is indicated for cases of STE-MI and none for non- STE
MI)
-
7/27/2019 3.2. Medicine_Acute Coronary Syndromes 2014A
2/4
JMA-1, JMA-2, Telma | Claveria Page 2 of4
Blood Testo Serum troponin I or T levels (or CK-MB if troponin not available)o Full blood counto Serum creatinine (eGFR) and electrolyte levelso Serum creatinine kinase (CK) levelo Serum lipid levels within 24 hourso Blood glucose level (to rule out co-morbidities)
Chest Xrayo Useful, but should not delay reperfusion treatment where indicated
(can be useful if there is congestion, patient can go on heart failure; orpresence of wide mediastinum indicating a dissecting aneurysm)
Caridac Biomarker: Troponin level (Cardiac Troponin I or T)o On arrival; + if pain is >3 hours (Not repeated if positive)o Repeat after 8 hours after last episode of pain or other symptoms of
coronary insufficiency if initially negative, then if 2nd test is still (-),
send patient home unless there is strong sign that patient has MI.
o Serial troponin measurements in patients with NSTEACS suspected tobe at high risk
Total CK Levelo Serial measurements performed for 48 hours in patients with MI. Can
be remeasured to confirm a second event if reinfarction is suspected
later
CK-MB Levelo Measure in all patients with an ACS if troponin assay unavailableo Troponin: goes up 24 hrs remains elevated up to 7 days CKMB: rise and
fall within 24 hrsINVESTIGATION (SUBSEQUENT)
Echocardiographyo Although acute STEMI cannot be distinguished from an old myocardial
scar or from acute severe ischemia by echocardiography, the ease and
safety of the procedure make its use appealing as a screening tool in
the Emergency Department setting.
o Echocardiographic estimation of left ventricular function is usefulprognostically
Radionuclide Scintigraphyo Myocardial perfusion imaging with 201Tl or 99mTc-sestamibi, which
are distributed in proportion to myocardial blood flow and
concentrated by viable myocardium, reveal a defect ("cold spot") in
most patients during the first few hours after development of a
transmural infarct.o Used less often than echocardiography because they are more
complicated and lack sensitivity and specificity in many clinical
circumstances
Cardiac Catheterization Cardiac MRIo Myocardial infarction can be detected accurately with high resolution
cardiac magnetic resonance imaging using a technique referred to as
late enhancement
o A standard imaging agent (gadolinium) is administered and images areobtained after a 10-min delay.
ECG CHANGES IN ACS
Figure 5. ECG changes/ injury pattern in MI : Q-wave remains
permanent. When a patient has a Q-wave, it can be said that there
was a previous MI
Ischemia (1-2 hours)oAbnormal Q waves >2mm wide or > 25% height of R wave in that lead
Unstable Angina/ NSTEMIoST-segment depressionoT-wave inversion in 30-50% of patients
ST-Elevation MIoST-segment elevation O.ooPathologic Q waveo Inversion of T wave
Figure 6. NSTEMI:Again, NSTEMI include MIs with T-wave inversion
or ST Depression
BIOMARKERS
Figure 7. Biomarkers of MI. The Troponins are the biomarker of
choice after 4 days, as they remain elevated for up to 10 days,
whereas CPK would have already gone down by Day 2). CPK goes up
within a few hours after an MI, peaks in 24 hours, and normalizes in
2 days.
Application: A patient comes in with ischemia that eventually
resolved. 5 days later, he had chest pain. What would you test for?
CPK! Troponin would still be up from the previous attack and will not
say anything about the recent one.
ASSESSMENT AND TREATMENT OF ACS Initial Assessmento Rapid but detailed inquiryo Vital signs and PEo 12-Lead ECG and Serial ECGo Chest X-rayo Enzymatic Assessment
Initial General Treatment (MONA)o Morphine: pain killer 2-4mg/ 5-10 min; SubQo Oxygen: 4L/mino Nitroglycerin: Sublingual or IVo Aspirin: 160 325 mg (Chew)
Note: Today, Statins are also used to establish pleopmorphic effect because
they have anti-oxidant effect which can fight against free radicals produced
by inflammatory processes.
-
7/27/2019 3.2. Medicine_Acute Coronary Syndromes 2014A
3/4
JMA-1, JMA-2, Telma | Claveria Page 3 of4
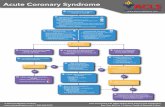
Figure 8. Treatment of ACS. Antiplatelets and anticoagulants are
important! When a patient comes in acutely complaining of chest
pain, we can be aggressive with treatment by opening up the
coronary a. to prevent further necrosis of cardiac cells- do a PrimaryPercutaneous Coronary Intervention (PPCI), preferably within 90
mins!
(For details about PCI, check out Ischemia trans)
SPECIFIC TREATMENT Reperfusion therapy: only for patients with ST segment elevation or new
Left Bundle Branch Block
Thrombolytic agents: (door-to-neddle time < 30 mins); for reperfusiontherapy
Kinases (e.g. Streptokinase) - dissolves thrombus unlike anticoagulantsthat only prevents thrombus formation. Acts by promoting the conversion
of plasminogen to plasmin which subsequently lyses fibrin thrombi.
Primary Percutaneous Transluminal Coronary Angioplasty (door-to-dilatation time < 60 mins)
o Effective in restoring perfusion in STEMI when carried out on anemergency basis in the first few hours of Mi
o It has the advantage of being applicable to patients who havecontraindications to fibrinolytic therapy.
CONTRAINDICATIONS TO USE OF THROMBOLYTICSA. Absolute Contraindications
History of Cerebrovascular Hemorrhage or CVA Non-hemorrhagic stroke or cerebrovascular event within the past
year
Marked hypertension (systolic > 180 mmHg and/or diastolic >110mmHg)
Suspicion of aortic dissection Active internal bleeding (including menstruation)
B. Relative Contraindications
Current use of anticoagulants A recent (10 min) cardiopulmonary resuscitation Known bleeding diathesis, pregnancy, a hemorrhagic Ophthalmic
condition (e.g., hemorrhagic diabetic retinopathy)
Active peptic ulcer disease History of severe hypertension that is currently adequately
controlled.
COMPLICATIONS OF THROMBOLYTIC USE Allergic Reactions Hemorrhage Hemorrhagic StrokeOTHER TREATMENTS OF ACS Conjunctive therapy: combined with thrombolytic agentso Aspirino Heparino Clopidogrel, potent antiplatelet agent
Adjunctive therapies - Agents given instead of or in addition tothrombolytic agents:
o IV Nitroglycerino Beta blockerso ACE inhibitors - especially in: Large infarction, Heart failure and
Hypertension
COMPLICATIONS OF ACUTE MI Earlyo Arrhythmiaso Acute Heart Failureo Cardiogenic Shocko Acute Mitral Regurgitationo Ventricular Septal Rupture or Free Wall Ruptureo Acute Pericarditiso Mural thrombosiso Sudden Death
Lateo Dresslers syndrome (fever, joint pain, pleurisy, pericarditis ) has a
dramatic response to Indomethacin or corticosteroids)
o Myocardial aneurysm and thrombuso Ischemic cardiomyopathyo Ventricular Fibrillation
Figure 9. Complications of Myocardial Infarction
CORONARY ARTERY DISEASE
-
7/27/2019 3.2. Medicine_Acute Coronary Syndromes 2014A
4/4
JMA-1, JMA-2, Telma | Claveria Page 4 of4
Figure 10. Course of Atherosclerosis. End-result is Coronary
Thrombosis
Initiated by rupture of an unstable plaque which leads to Coronary a.Occlusiono Intermittent Occlusion= Unstable AnginaoComplete occlusion= Acute MI
3 Is of coronary artery event: Ischemia, Injury, InfarctionUNSTABLE ANGINA/ NSTEMI
Most commonly caused by a reduction in oxygen supply and/ or by anincrease in myocardial oxygen demand superimposed on an
atherosclerotic coronary plaque, with varying degrees of obstruction.
Four pathologic processes that may contribute to the development ofUA/NSTEMI:
o Plaque rupture or erosion with superimposed non-occlusive thronmbus(most common cause)
o Dynamic obstruction (eg. coronary spasm, as in Prinzmetals/ variantangina)
o Progressive mechanical obstruction (rapidly advancing coronaryatherosclerosis or restenosis following percutaneous coronary
intervention)
o Secondary UA related to increased myocardial oxygen demand and/ordecreased supply (eg. tachycardia, anemia)
Progressioin of Myocardial Infarctiono Acute Stage: First few hours to 7 dayso Healing Stage: 7-28 dayso Healed Stage: >29 days