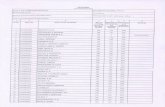
P. de LEY 186 - Requisitos Ambientales Para Construcción de Carreteras
186-P
Transcript of 186-P

185-P DEDUCTION OF MISMATCHED DONOR HLA FROM URINE SAMPLES OF KIDNEY TRANSPLANTED RECIPIENTS.Ricky Lau 1, Janette Kwok 1, Gavin Chan 2, K.T. Tam 1, M.F. Lam 3, Maggie Mok 3, W.L. Chak 4, Cheuk Au 5, K.W.Chan 2, K.F. Chau 4, Matthew Tong 5, T.M. Chan 3. 1 Transplantation and Immunogenetics, Queen Mary Hospital,Hong Kong SAR, China; 2 Department of Pathology, Queen Mary Hospital, Hong Kong SAR, China;3 Department of Medicine, The University of Hong Kong, Hong Kong SAR, China; 4 Department of Medicine,Queen Elizabeth Hospital, Hong Kong SAR, China; 5 Department of Medicine & Geriatrics, Princess MargaretHospital, Hong Kong SAR, China.
Aim: We previously demonstrated that mismatched donor human leukocyte antigen (HLA) could bededuced from HLA typing of fresh or archived paraffin-embedded renal allograft tissue (Clin. Transplant2010;24:E178-81; Histopathology, In press), thereby allowing the detection of donor-specific antibodies. Inthe present study, we investigated the detection of mismatched donor HLA using the kidney recipient’s urinesample.
Methods: Forty-three urine samples from kidney transplant recipients with known HLA in both donor andrecipient were studied. Each 40 ml sample was centrifuged at 2500 rpm for 20 minutes. The supernatant wasdiscarded, the sediment washed with 1X PBS, after which the mixture was centrifuged at 2500 rpm for20 minutes. DNA extraction was performed on samples with sufficient cell sediment through visual inspec-tion. Genomic DNA was extracted using EZmag Genomic DNA Whole Blood Kit (Texas BioGene Inc., Taiwan).HLA Class I and II antigens were typed by PCR-SSP.
Results: 62.8% (27/43) of urine samples showed sufficient sediment. Extracted DNA concentration was inthe range of 1700-2600 gg with purity (A260/A280) of 1.66-1.98. 41.9% (18/43) had sufficient DNA for HLAtesting. One case had zero mismatch between donor and recipient. Of 17 mismatched cases, the HLA typingof recipients was achieved in all subjects. Mismatched donor HLA phenotypes were detected completely in 3of the 17 subjects (17.6%), with the samples collected on Day 5, 14, and 1268 after kidney transplantation.Mismatched donor HLA data was partially detected in another 6 subjects (35.3%).
Conclusions: Detection of mismatched donor HLA from the urine of kidney transplant recipients has anoverall success rate of 7% (3/42). The presence of sufficient donor-derived substrate for HLA typing appearscritical. Further investigations are warranted to explore ways to improve the performance of this non-invasivetechnique for the detection of mismatched donor HLA in kidney transplant recipients with unknown donorHLA phenotype.
186-P STORAGE OF DNA ON FILTER PAPER: QUALITY TEST ON SAMPLES KEEPING 10 YEARS. Victoriano J. Leon 1,Alberto J. Leon 2, Amador Crego 1. 1 Servicio de Analisis Clinicos, Hospital Universitario de Salamanca,Salamanca, Spain; 2 Division of Experimental Therapeutics, Toronto General Research Institute, Toronto, ON,Canada.
Aim: The creation of a registry of samples of genomic material, usually requires a painstaking process toobtain the DNA and to store it at �85 �C. All this implies a high cost in terms of staff, material, and storage,which limits the size and the number of archives. The conservation of blood samples (or previously extractedDNA) on filter paper allows a great number of samples to be held within a small space without any mainte-nance, making it very easy to access the DNA of the sample and carry out different genomic studies, especiallythose that use PCR technique.
Methods: Several samples of 25 mcl of blood, or DNA previously extracted, on Whatman no 3 paper, anddried at room temperature or in a heater at 45 �C. Insert the filter paper of the sample into an envelopeand label it. Enclose several of these envelopes within, in a plastic bag with hermetic closing and silica geldesiccant and keeping ten years. The spot on the filter paper for study is cut and placed in an Eppendorf tube,200 mcl of a 4 M solution of guanidine isotiocianate is added, and it is then heated at 55 �C for 30 minutes. TheDNA released from the paper can be extracted either with saline precipitation, phenol chloroform or cationicresins. The technique we have chosen was the Kit Direct II of Dynal, due to its ease and rapidity; it is based ona resin with a metallic core which permits the separation of the DNA-resin complex with an magnetic con-centrator, and the complex is undone at 65 �C for 5 minutes. After removing the imam with the resin, DNAin a liquid phase remains at a quantity of 1-4 mcg, ready to be employed. We have applied the DOP-PCR tech-nique, when the amount of DNA available in a blood spot is not enough for our porpoises, such as a completeHLA genomic study.
Results: We have stored our samples over filter paper for periods of over ten years, using the DNA restoredfor the genomic typing of HLA class I and II, and also for coagulation factors.
Conclusions: Satisfactory results in all the cases.
Abstracts / Human Immunology 73 (2012) 49–167 165