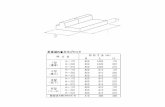
Spare Parts List - haute pression...Spare Parts List ICA Ref: IDAF40229 - . Model: ROYAL P.170 TRi
170-P
Transcript of 170-P
170-P ALTERNATIVE TO 8/8 MATCHED DONORS - A CASE STUDY. Lisa Harper, Teri Steeves.. HistocompatibilityLaboratory, Hamilton Healtch Sciences, Hamilton, ON, Canada.
Aim: As fewer sibling marrow donors are available due to decreasing birthrates, alternatives are more fre-quently being considered when 8/8 matched allele donor for HLA-A,B,C,DRB1 are not available & clinically,recipient needs urgent transplant. Our current Bone Marrow Policy includes consideration of single mismatch& single haplotype matched donors. Antibodies directed against donor specific antigens (DSA) are avoided toreduce the risk of graft failure. This case demonstrates the need for additional typing beyond policy whenantibodies were identified.
Methods: Patient: 59 Y/O female, AML Initial typing performed by SSP at HLA-ABCDRB1, no related donors,high resolution typing performed and unrelated search initiated. No 8/8 matches identified. Two potential 7/8unrelated registry donors were selected, samples sent to us for high resolution and DQB1 typing. Antibody IDwas performed using Luminex with OneLambda Single Antigen on recipient’s serum.
Results: Antibodies were identified in the recipient’s serum to Class I & II antigens. No DSA’s were identi-fied to either of the mismatched class I donor antigens. DRB3⁄01:01 & DRB3⁄03:01 Class II antibodies wereidentified. Additional high resolution typing of the recipient & donor’s DRB3⁄ (not normally required) wasperformed to determine DSA status. Recipient & donors typed as DRB3⁄02:02, therefore the antibodies werenot DSA. Donor was selected & transplant booked for April 19, 2013.
Conclusions: When a fully matched donor is not available for a patient and the clinical status of the patientindictes the need to continue to transplant then alternatives must be considered. Our transplant program ismoving in the direction of related single haplotype matched transplants and single mismatch antigen/alleleunrelated donors while ensuring that DSA is not identified against the mismatched antigen(s)/alelle(s). Addi-tional urgent laboratory testing & investigation beyond our standard testing process is required to ensure themost suitable donor is selected.
171-P VIRTUAL CROSSMATCHING: IT’S NOT AS SIMPLE AS IT SEEMS. June Jones, Julie Houp, Alyson Morris, AnnetteJackson, Mary Leffell, Andrea Zachary. Immunogenetics, Department of Medicine, Johns Hopkins University,Baltimore, MD, USA.
Aim: Use of the virtual crossmatch (XM) has increased the efficiency of organ allocation and reduced thenumber of organs declined based on unexpected positive XMs (Cecka JM., et al. Am J Transplant. 2011).Despite these benefits, a cell based XM still provides a final safeguard before transplantation. False negativeXM predictions may arise when reactivity is due to both antigen specific antibodies and antibodies to cross-reactive epitopes.
Methods: HLA-specific antibodies were assessed using class I or class II phenotype panels and IgG or C1Qsingle antigen bead assays. (Lifecodes Immucor; Labscreen, One Lambda,Inc). One wash CDC B cell XMs wereperformed.
Results: Luminex IgG tests yielded reactivity with DR53 phenotypes ranging from 3,000-10,000 MFI withDR53 heterozygotes and >10,000 MFI with homozygotes. Reactivity with DR10 phenotypes were 2,000-3,000MFI. Single antigen beads yielded reactions with DR53 of 20,000 MFI with undiluted serum and 17,000 MFIwith serum diluted 1:8. Reactions with DR10 were 15,000 and 2,000 MFI with undiluted and 1:8 dilutedserum, respectively. MFI values given above would predict negative XMs with DR10+/DR53- cells and positiveXMs with DR10-/DR53+ cells. The C1q assay yielded MFI values of 28,000 with DR53 and 300 with DR10.These C1Q results substantiate the prediction of a negative CDC XM result with a DR10 cell. CDC XM testsyielded the following results: + with a titer of 2 with a DR10+/DR53- cell, + with a titer of 32 with aDR10-/DR53 homozygote cell, and negative with DR53 heterozygotes and with cells bearing other antigenscrossreactive with DR10 (DR1 and DR15/51).
Conclusions: We propose that the CDC+ XM with the DR10 cell was due to contributions from the DR10antibodies and the much stronger antibodies to DR53 that shares one or more epitopes with DR10. These datashow that accurate prediction of crossmatches must take into account the possible contributions of antibodiespositive for antigens crossreactive with the target antigen.
Abstracts / Human Immunology 74 (2013) 51–173 163









![FABCO PTO-170-23 ENGINEERING REPORT · 2020. 2. 19. · fabco automotive corporation . engineering short form report m 873-0039-003/p-c -873-0039-003 -pto-170-23. rev [ ] drawing](https://static.fdocuments.us/doc/165x107/60cd1df65094d41a7d26c6eb/fabco-pto-170-23-engineering-report-2020-2-19-fabco-automotive-corporation.jpg)









