152 Inter-treatment compensation of treatment setup variation to enhance the radiotherapeutic ratio
Transcript of 152 Inter-treatment compensation of treatment setup variation to enhance the radiotherapeutic ratio

Proceedings of the 37th Annual ASTRO Meeting
152 I N T E R - T R E A T M E N T C O M P E N S A T I O N O F T R E A T M E N T SETUP VARIATION T O ENHANCE T H E RAD1OTI tERAPEUTIC R A T I O Di Yah*, D.Sc., John Wong*, P h D , JeffMichalski a, M D , Cheng Pan*, Ph D , Arthur Frazier*, M.D, Walter Bosch a, D .Sc and Alvaro Marfinez*, M . D FACR. *Department o f Radiation Ontology William Beamnont Hospital, Royal Oak, M1 aMallinckrodt Institute of Radiology. Washington University School of Medicine, St. Louis, MO
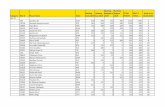
Purpose; In radiotherapy, treatment setup error has been one of the major causes of dose variation in the treated volume, With the data acquired from on-line electronic portal imaging, it is now possible not only to adjust the patient setup, but also to modify the treatment plan during the course o f clinical treatment based on the setup error measured for each individual patient, in this work, daily clinical portal images were retrospectively analyzed to study (1) the number of initial daily portal images required to give adequate prediction of the systematic and random deviations of treatment setup, and (2) the potential therapeutic gain when the inter-treatment planning modification was established using the setup error of each individual patient. Methods a n d Mater ia ls : Only those patients whose treatment positions had not been adjusted during the course o f treatment were selected for the retrospective s tudy Daily portal images of 27 lung, 25 pelvis, and 12 head and neck (h&n) cancer patients were obtained from two independent clinics with similar setup procedures. The anterior-to-posterior field was analyzed for the pelvis and lung treatments, and the right lateral field for the h&n treatments Between 13 to 30 daily portal images were acquired for each patient and were analyzed using a 2D alignment too l Systematic and random deviations of the treatment setup were calculated for each individual patient. The statistical confidence on the convergence of both systematic and random deviations with time were tested to determine the number of initial daily portal images needed to predict these deviations. In addition, a mean deviation for each site was also calculated using the setup errors from all patients Two treatment planning schemes were simulated to evaluate margin design and prescription dose adjustment Therapeutic scores were quantified in terms of tumor control probability (TCP) and normal tissue complication probability (NTCP) In the first planning scheme, a uniform margin based on the mean deviation and fixed prescription dose were used t'or all treatment plans In the second, the same margin and prescription dose were used only for the initial planning. These were adjusted, by reducing the treatment field margin and escalating the prescription dose, whenever necessary in order to improve the therapeutic scores of the initial plan Results: For those patients whose setup variations did not drift with time, the systematic and random deviations for the treatment course were found to be within +_1 ram for the former and +_0.5 mm for the latter at _> 90% confidence level using <_ 8 initial daily portal images. Six pelvic patiems and three hmg patients exhibited the setup error that drifted with time and required more frequent portal image vedficaLion The distribution of setup errors for the individual patients deviated from the mean deviation by 47 , 2 1 and 1.5 ram, for the treatment of pelvis, lung and h&n respectively. These values were used to determine thresholds when the margin and prescription dose need to be modified on an individual patient basis. Our results show that dose could be escalated safely in at least 80% of the pelvis treatments, 63% of tile lung treatments and 41% of h&n treatments if the inter- treatment modification is used. These will increase the TCP about 15% for the lung treatment, 18% for the pelvis treatment, and 4% for the h&n treatment with the NTCP at the same level Conclusion: Our work demonstrates a different approach for the use of on-line portal images This approach focuses on modification of the treatment plan, rather than treatment setup adjustment. Our results show the potential to improve the therapeutic ratio based upon feedback from the initial radiation treatments This strategy can help direct the modification o f both the prescription dose and treatment margin, leading to individually optimized dose escalation of conformal therapy
217
153
E V A L U A T I O N OF T H E A C C U R A C Y O F A M E T H O D F O R AUTOMATIC P O R T A L I M A G E R E G I S T R A T I O N
Daniel S. Fritsch 1'2, Edward L. Chancy t, Matthew J. McAuliffe 2, Suraj Raghavan 2, Aziz Boxwala 2. John R.D. Earnhart ~
IDeparmaent of Radiation Oncology, 2Depar~ent of Biomedical Engineering. The University of North Carolina, Chapel Hill, NC
Purpose/Object ive: Portal imaging is the most important quality assurance procedure for monitoring the precision of radiation therapy in standard ctinical practice and is even more essential for monitoring the highly-customized and technically-demanding fields derived from 3D treatment planning. Unfortunately, traditional methods for acquiring and interpreting portal images suffer from a number of deficiencies which contribute to the we l l documented observation that many setup errors go undetected and some persist for a elinica~y significant portion of the prescribed dose. We have developed a technique called core analysis for the automatic extraction of anatomical structures and have developed robust, automatic means for registering portal images via correspondence of computer-extracted, core-based fiducial curves. Core analysis is a fundamental computer vision method that automatically finds the geometric middles and associated widths of objects in digital gray-scale images. The corer of stable anatomic features (e.g., bOnes) can in turn serve as fiducial structures for on-line automatic registration of digital portal images with a gold standard reference image (e.g., DRR or digitized simulation film). The robustness of our tectmique derives from the invarlano© of core-based extraction of fiduvials to translation, rotation and zoom and the insensitivity o f cores to noise and blurring,
Mater ia ls & Methods: A significant shortcoming of the analysis of portal registration techniques reported in the literature is 10ck of knowledge of truth for clinical images. While careful use of phantoms provides meastucs of accuracy, lack of realism leaves serious doubts as to the expected clinical reliability. As an extension of our 3D treatment planning system we have developed a method for producing realistic megavoltage portal radiographs with exactly-known setup errors. We have used this software to produce simulated porter radiographs for a number of treatment sites to test the accuracy and precision of our registration method. For example, a series of 20 simulated portal images with random field positioning errors of :15 n'an in translation and _+.5 ° in rotation were used to evaluate the accuracy of core-based portal image registration for a patient undergoing u'eatment for prostate cancer. In a one-irene preprocessing step, fiducial cores were generated for user-selected anatomical structures (bones) in a reference potful image and were automatically generated for each of the images containing known positioning errors via a core-based object recognition approach that takes into account both position and width information given by the cove.
Results: For the pelvic study, in all cases the reported translation was within 1 mm of the actual translation with mean absolute errOrs in tranalation of 0.3 mm and standard deviations of 0.3 ram. In all cases the reported rotation was within 0.6 ° of the actual rotation with a mean absolute error of 0.18 ° and a standard deviation of 0.23 ~. While this study does not directly extrapolate to the clinical setting, sinoc no non-rigid patient motion was allowed, the accuracy and precision serve as a benchmark to measure registration performance and to compare different means (both interactive and automatic) for verifying treatment se tup
Conclusions: Both the accuracy and precision of our automatic portal registration technique have been measured for a number o f cases including a prostate AP field using elmicaUy-matisfie, simulated portal radiographs with exactly.known positioning errors. Automatic analysis of other treatment sites using simulated portal images generated from the NLM Visible Human datasets have demonstrated comparable results indicating acceptable performance of our methods for routine clinical use.