1.1 Clinical Presentations of Rheumatic Disease in Different Age Groups - The_child_patient
description
Transcript of 1.1 Clinical Presentations of Rheumatic Disease in Different Age Groups - The_child_patient
-
The child patient
Page 1 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
Publisher: OxfordUniversityPress PrintPublicationDate: Oct2013PrintISBN-13: 9780199642489 Publishedonline: Oct2013DOI: 10.1093/med/9780199642489.001.0001
Chapter: ThechildpatientAuthor(s): LoriB.TuckerDOI: 10.1093/med/9780199642489.003.0001
OxfordMedicineOnline
OxfordTextbookofRheumatology(4ed.)EditedbyRichardA.Watts,PhilipG.Conaghan,ChristopherDenton,HelenFoster,JohnIsaacs,andUlfMller-Ladner
LatestupdateInNovember2014,80chapterswereupdated.NumerousupdateshavebeenmadeincludingtothechaptersonRheumatoidArthritis,theGeneticsandEnvironmentsection,theManagementsection,andmuchmore.WealsowelcometwonewauthorsSebastienViatteandCharlesRaine.
Thechildpatient
IntroductionMusculoskeletalcomplaintsinchildrenareverycommon,andmostaregenerallyinconsequentialandself-resolving.However,itisimportanttodifferentiatechildrenwithminorproblemsfromthosewhohavedevelopedamoreseriousmusculoskeletalproblempossiblyassociatedwithlong-termillness.Thisisfrequentlychallengingtotheclinician,asthedifferentialdiagnosisofconditionsassociatedwithmusculoskeletalcomplaintsisbroadandchildrenpresentspecialcircumstancestoconsider.Thespectrumofchildhoodrheumatic
-
The child patient
Page 2 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
diseasesisshowninTable1.1.Afulldiscussionofchildhoodrheumaticdiseasesisbeyondthescopeofthischapter;summariesofmanyoftheimportantdiseasesareprovidedinlaterchaptersorothersources.
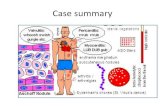
Table1.1Thespectrumofchildhoodrheumaticdisease
JIA
SLE SLENeonatalLE
Juveniledermatomyositis
Scleroderma Limitedorlocalized:morphea,linear,generalizedcutaneousSystemicsclerosis
Vasculitides KawasakidiseaseHenochSchonleinpurpuraGranulomatouspolyangiitisTakayasu'sarteritisPolyarteritisnodosa
Granulomatousdisease Sarcoidosis
Acuterheumaticfever
Autoinflammatorydiseases
PeriodicfeversyndromesCRMO
CRMO,chronicrecurrentmultifocalosteomyelitis;JIA,juvenileidiopathicarthritis;LE,lupuserythematosus;SLE,systemiclupuserythematosus.
ClassificationsofrheumaticdiseaseinchildrenTheclassificationofarthritisandotherrheumaticdiseasesinchildrenhasposedsignificantchallenges,anduntilrecently,theuseofdifferentclassificationsystemsforthemostcommonrheumaticcondition,arthritis,resultedininabilitytocompareresearcharoundtheworld.
Classificationofchildhoodarthritis
Theclassificationofchildhoodarthritishasevolvedoverthepast10yearssincethepublicationoftheInternationalLeagueofAssociationsforRheumatology(ILAR)criteriaforjuvenileidiopathicarthritis(JIA)in2002. Thesecriteriaweredevelopedbyaninternationalcommitteeofpaediatricrheumatologists,usingexpertopinion,aswellasaconsensusprocess
1
2
-
The child patient
Page 3 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
andevidence-basedmodifications.Beforethesecriteriaweredeveloped,childrenwerediagnosedusingeithertheAmericanCollegeofRheumatology(ACR)criteriaforjuvenilerheumatoidarthritis ortheEuropeanLeagueAgainstRheumatism(EULAR)criteriaforjuvenilechronicarthritis; theuseofthesedifferingcriteriasetsledtodifficultyincomparingpatientcohortsacrossdifferentcountriesandpublications(Table1.2).
Table1.2Comparisonofcriteriaforchronicarthritisinchildhood
ILARcriteria(JIA) ACRcriteria(JRA) EULARcriteria(JCA)
OligoarthritisPersistentExtended
Pauciarticular Pauciarticular
PolyarthritisRF Polyarticular PolyarticularRF
PolyarthritisRF+ PolyarticularRF+
Systemicarthritis Systemic Systemic
Psoriaticarthritis Psoriatic
Enthesitis-relatedarthritis Ankylosingspondylitis
Undefinedarthritis
JCA,juvenilechronicarthritis;JIA,juvenileidiopathicarthritis;JRA,juvenilerheumatoidarthritis;RF,rheumatoidfactor.
ThereisnowmorewidespreadadaptationoftheILARcriteriaforchildhoodarthritisworldwide.Theoveralltermjuvenileidiopathicarthritis(JIA)isdefinedasdefinitearthritisoccurringbeforethe16thbirthday,persistingforatleast6weeksandofunknowncause.TherearesevencategoriesofJIAdefinedbytheILARcriteria(Table1.3).Ofimportance,theILARcriteriaincludeacategoryofenthesitis-relatedarthritis(ERA)whichencompasseschildrenpreviouslydescribedashavingspondyloarthropathy,seronegativeenthesitisandarthropathy,andjuvenileankylosingspondylitis.Therehasbeencontroversyregardingtheuseofafamilyhistoryofpsoriasisasanexclusioncriteriaforsomesubtypes,andsomedifficultiesofclassificationinthesubtypesofpsoriatic,ERA,andunclassifiedJIA.
Table1.3ILARcriteriafortheclassificationofjuvenileidiopathicarthritis
Category Definition Exclusions
Oligoarthritis Arthritisinlessthan5jointsduringthefirst6monthsofdiseasePersistent:nevermorethan4joints
1,2,3,4,5
34
24
4
2
-
The child patient
Page 4 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
Persistent:nevermorethan4jointsExtended:morethan4jointsafterthefirst6monthsofdisease
PolyarthritisRF+
Arthritisin5ormorejointsduringthefirst6monthsofdisease,withpositiveRFtest(X2)
1,2,3,5
PolyarthritisRF
Arthritisin5ormorejointsduringthefirst6monthsofdisease,withnegativeRFtest
1,2,3,4,5
Systemicarthritis
Arthritiswithfeverof2weeks'duration,documentedtobequotidianforatleast3days,andaccompaniedbyoneormoreof:
(a)evanescent,non-fixedrash(b)hepatomegalyorsplenomegaly(c)serositis(d)generalizedlymphadenopathy
1,2,3,4
Psoriaticarthritis
Arthritisandpsoriasis,orArthritiswithoneormoreof:
(a)dactylitis(b)nailpittingoronycholysis(c)psoriasisinafirstdegreerelative
2,3,4,5
ERA Arthritisandenthesitis,orArthritisorenthesitiswithoneormoreof:
(a)sacroiliacjointtendernessand/orinflammatorylumbosacralspinalpain(b)HLAB27positivity(c)acutesymptomaticuveitis(d)first-degreerelativewithHLAB27associateddisease(e)onsetofarthritisinaboyovertheageof8years
1,4,5
Undefinedarthritis
Achildwitharthritiswhomeetscriteriaformorethanonecategoryorfornocategory
ERA,enthesitis-relatedarthritis;RF,rheumatoidfactor.Exclusions:
1.Psoriasisinthepatientorfirst-degreerelative.
2.ArthritisinanHLAB27positivemalewithonsetafter8yearsofage.
3.Anklyosingspondylitis,enthesitis-relatedarthritis,sacroilitiswithinflammatoryboweldisease,Reiter'ssyndrome,oracuteanterioruveitisinafirst-degreerelative.
-
The child patient
Page 5 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
4.PresenceofIgMRFonatleasttwooccasionsmorethan3monthsapart.
5.ThepresenceofsystemicJIA.
Classificationsofotherchildhoodrheumaticconditions
Theonlydiagnosticcriteriawhichhavebeendevelopedspecificallyforclassificationordiagnosisofchildhoodrheumaticdiseasesarethoseforacuterheumaticfever andforKawasakidisease. Bothofthesecriteriasetshavereasonablyhighsensitivitybutlowerspecificity.Specifically,strictapplicationoftheKawasakidiseasecriteriawillexcludechildrenwhohavewhatisdescribedasatypicalKawasakidisease'.Thesechildrendonotfulfilthepublishedcriteria,butareathighriskfordevelopmentofcoronaryarteryaneurysmsandpooroutcome.
Criteriaforthediagnosisofmostotherchronicrheumaticdiseasesofchildhoodhavegenerallybeenadoptedinwholeorpartfromclassificationcriteriaforadults.Forexample,theclassificationcriteriaforsystemiclupuserythematosus(SLE) anddermatomyositis areusedingeneralpracticeforthediagnosisoftheseconditionsinchildren.However,recentworkhasbeendonetoexaminethevalidityofclassificationcriteriaforsystemicvasculitidessuchasHenochSchonleinpurpura,polyarteritisnodosa,Takayasuarteritis,andgranulomatouspolyangiitis(formerlyknownasWegener'sgranulomatosis )forchildren.In1990,consensuscriteriadefinitionswereproposedbyagroupofexpertrheumatologistsfromtheACRforthesevasculitisconditions. In2008,aninternationalpaediatricrheumatologyconsensusconferencewasconvenedtovalidateandfinalizepaediatricvasculitisdiagnosticcriteria;usingstandardconsensusformationmethodologyandpatientcasedata,finalizedclassificationcriteriawerepublishedwhichdemonstratedhighsensitivityandspecificityintheseexercises.
EpidemiologyofchildhoodrheumaticdiseasesItisacommonmisconceptionthatrheumaticdiseasesarerareinchildhood.Infact,chronicarthritisisoneofthemostcommonchronicconditionsofchildhoodassociatedwithdisability.Inaddition,asignificantpercentageofpatientswithautoimmunediseasessuchasSLEhavedevelopedtheonsetofdiseaseinchildhood.Somerheumaticdiseasessuchasdermatomyositisandlocalizedsclerodermaaremorefrequentinchildrenandadolescentsthaninadults.SomediseasessuchasoligoarticularJIAwithuveitis,systemicJIA,acuterheumaticfever,HenochSchonleinpurpura,andKawasakidiseaseoccuralmostexclusivelyinchildhood.Conversely,thereareanumberofrheumaticdiseasesthatrarelyoccurinchildhood,includinggout,calciumpyrophosphatedepositiondisease,polymyalgiarheumatica,andprimaryosteoarthritis.
Accuratedatademonstratingtheincidenceandprevalenceofchildhoodarthritisissurprisinglysparse.Muchofthedataavailablehascomefrompaediatricrheumatology-basedclinicpopulationsorregistries,whichmayresultinunder-reportingofthetruefrequencyofdisease.ThemostcurrentinformationsuggeststhattheprevalenceofJIAisbetween10and400per100000children,dependingongeographiclocationandcasedefinitions. Of
56
7,8 9
10
11,12
11,13
14
15
-
The child patient
Page 6 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
interest,apopulation-basedstudybyMannersandDiepeveen suggeststhattheprevalenceofchronicarthritisin12-year-oldAustralianchildrenwasactuallymuchhigherthanexpected(400/100000).ReportedincidenceofJIArangesfrom1to2per100000children,withmostreportscomingfromclinic-basedstudiesinEuropeorNorthAmerica. Asurveillance-basedstudyfromCanadadonein20072009foundacalculatedincidencerateof4.3per100000children; howeverthisislikelytobeanunderestimateascaseswerereportedbypaediatriciansonly.
Accuratefrequenciesoftheotherchildhoodrheumaticdiseases,suchasSLE,dermatomyositis,scleroderma,andvasculitis,areevenmoredifficulttofind.Population-basedstudiesusingadministrativedatahavenotbeendoneinthesepopulations.
Ageandsexdistributionsoftherheumaticdisordersofchildhooddifferbydisease.Forexample,SLEismorecommoningirlsthaninboys,andfarmorefrequentinchildrenoverage10years.OligoarticularJIAismorecommoningirlsyoungerthanage6years,andERAmorecommoninboysoverage6years.However,theserules'arenothardandfast,andcliniciansneedtobeawarethatrheumaticdiseasecanpresentinchildrenasyoungas1yearofage.
Ethnicvariationoccursinsomechildhoodrheumaticdiseases.JIAisfoundaroundtheworld,butthedistributionofdiseasesubtypeshasbeenreportedtodifferindifferentcountries.Forexample,JIAsubtypedistributioninIndiaisquitedifferentfromthatinNorthAmerica.
InteractionofgrowthanddevelopmentwithchildhoodrheumaticdiseasePhysicalgrowth
Oneofthemajordifferencesbetweenchildhood-onsetandadult-onsetrheumaticdiseaseisthepotentialeffectofhavingachronicinflammatorydiseaseonthenormalgrowthoftheaffectedchild.Thepresenceofactiveinflammationcanstuntthelineargrowthofanaffectedchild.Additionally,treatmentsusedforchronicinflammatorydiseases,mostnotablycorticosteroids,haveprofoundnegativeeffectsongrowth.Carefuldocumentationoftheheightandweightofachildwithrheumaticdiseaseshouldbemadeateachmedicalencounter,andcomparedtogrowthcurvesforhealthychildrenofthesamesexandage.Itisimportanttoconsiderthechild'sgeneticbackgroundandparentalheightsinassessinggrowthratesforanindividualchild.Serialmeasurementsensurethatgrowthvelocityovertimeisnormal.Growthratesmayincreasetoallowcatch-upgrowthoncediseaseiscontrolled;forexample,achildwithpoorlycontrolledJIAmayhaveagrowthspurtoncediseaseiscontrolledusingmethotrexate.However,somechildrenwillhavepermanentgrowthstuntingfromthecombinationofsevereactivediseaseandtherequirementforhighdosesofcorticosteroids.
Motordevelopment
Youngchildrenwhodeveloparheumaticdiseasemayhavedelayedmotordevelopmentduetotheirdisease.Forexample,averyyoungchildwhodevelopsJIAmaynotlearntowalkorjumpattheappropriatetimesduetopainandinabilitytomovejointsnormally.Recognitionoftherangeofnormaldevelopmentinyoungchildrenisessentialforinterpretationoffindingsonthephysicalexaminationandfunctionalassessment.Thereisconsiderablevariationinthe
15
16
17,18
19,20
-
The child patient
Page 7 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
ageatwhichindividualdevelopmentalmilestonesareachieved.ThedatesinTable1.4shouldbeusedasaguidelineonly.
Table1.4Normaldevelopmentalgrossmotormilestonesinchildren
Age(months) Milestonesachievedbythisage
7 Independentsitting
10 Crawling
12 Cruising,walkingwithonehandheld
15 Walkingalone,crawlingupstairs
18 Runningstiffly
24 Runningwell;walkingupanddownstairsonestepatatime
30 Jumping
36 Walkingupstairsalternatingfeet,ridestricycle
48 Hoppingononefoot
60 Standingononefoot;skipping
Delayinachievingmotormilestonesmayoccurinachildwithanychronicdisease,butthismaybemoreevidentinthechildwithadiseaseaffectingthemusculoskeletalsystem,thefunctionofwhichisthebasisfortheestimationofdevelopmentalstages.Althoughtheremaybeadelayinthechronicallyillchild,milestonesareeventuallyachievedovertime.
Psychosocialdevelopment
Chronicillnesscanhaveamajorimpactonthequalityoflifeofthefamily,aswellasthechild,throughouttheirdevelopment.AsignificantnumberofchildrenwithJIAhavedisabilitythatinterfereswithfullfunctioningatsometimesduringchildhoodandadolescence,andchildrenwithserioussystemicrheumaticconditionssuchassystemiclupus,vasculitis,ordermatomyositismayhavemajorinterferencewithregularfunctioning.Forchildrenwithrheumaticdisease,careneedstobefamilyfocused,andisbestdeliveredbyamultidisciplinarypaediatricrheumatologyteamwhichoftenincludessocialworkersandpsychologists.
Educationalconsiderations
Theschoolisoneofthechild'smostimportantenvironments,andparticipationintheschool
-
The child patient
Page 8 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
environmentisastronginfluenceonhealthydevelopment.Attentiontoschoolperformance,bothacademicandsocial,iscriticaltopromotinghealthydevelopment.Childrenwithrheumaticdiseaseshouldbeexpectedtoparticipatefullyinschool,withmodificationsifnecessarytoaccountfortheirphysicalconsiderations,physicianvisits,ortreatments.Anassessmentofschoolattendance,participation,limitsandconcernsshouldbeapartofeveryfollow-upvisit.Directcontactbetweenthemedicalteamandthechild'steachersorcounsellorsisoftenbeneficialineducatingschoolpersonnelaboutthechild'sconditionanddesigningmodificationsthatareappropriate.Forexample,theuseofalaptopcomputerfortakingnotesandtestsmaybeimportantforthechildwitharthritisinvolvingthehandsandwrists.Childrenwithrheumaticdiseaseshouldbeencouragedtoparticipateinphysicalactivityatschool,suchasphysicaleducation,playtime,orsportsteams;routineproscriptionfromactivityisnothelpfulfortreatmentandleadstosocialisolationandgeneralizedpoorconditioning.
Aschildrenmoveintoadolescence,thedevelopmentaltrajectorybeginstoincludeissuesrelatingtoself-esteem,sexuality,peerrelationships,educationalandvocationalgoals,andindependence.Havingachronicrheumaticillnessoffersuniquechallengestotheadolescentandtheirparents,andthesupportandguidanceofaknowledgeablesubspecialtyteamisveryimportantthroughthistime.Thetimingoftransitionfromthepaediatrictotheadulthealthcaresettingvarieswiththepatient,family,physician,andhealthcaresetting.Ingeneral,adolescentswillbecaredforbythepaediatricrheumatologyteamuntilthetimeofcompletionofsecondaryeducation,andenteringtheworkforceorpost-secondaryeducation.Insomesettings,transitionclinicshavebeendevelopedtocareforyouthwithrheumaticdisease.Thegoalsofthesetransitionprogramsaretopromoteyouthindependenceinhealthcare,educateyouthabouttheirdiseaseandneeds,andpreparethemtomovetotheadulthealthcaresetting.
Sexualmaturation
Chronicinflammatorydiseasecanresultinadelayinsexualmaturation.Completegenitalmaturity(Tanner5)mayoccurbeforetheageof13years,butmaynotoccuruntilageof18years. Menarcheoccursatanaverageof1213yearsinNorthAmericaandEurope.Theonsetofmenstruationmaybedelayedingirlswithactiveinflammatorydisease;also,mensesmaybecomeirregularorceaseinagirlwhohaspreviouslyhadaregularmenstrualpattern.
Adelayinsexualmaturationmaybeasourceofanxietyforadolescents,andoftenthesepatientsmaynotbecomfortableraisingissuesofconcernregardingsexualitywiththemedicalteam,especiallyinthepresenceoftheirparents.Itisusefultohavesomepartofthemedicalvisitwiththeadolescentalone,andthephysicianornurseshoulddirectlyaddressissuesofsexualmaturityandfunctioningatthattime,whilereassuringtheadolescentoftheconfidentialityoftheconversation.Careshouldbetakentobecertainthattheadolescentunderstandsthecriticalaspectsofconversationsaroundmedicationsandteratogenicityorimpactonfertility.Forexample,thecommentYoucan'tgetpregnantwhiletakingcyclophosphamide'maybeinterpretedtomeanthattheadolescentdoesnotneedtousebirthcontrol,ratherthanbeingextremelycarefultoavoidpregnancy.
Assessment
21,22
23
-
The child patient
Page 9 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
Historyandphysicalexamination
Thehistoryandphysicalexaminationprovidemostofthediagnosticinformationinchildrenwithrheumaticdiseases;laboratorytestsprovidelittlehelp.Thehistoryshouldbeobtainedfromthechild'susualcaregiverifpossible(parentorotheradult),andthechild.Evenayoungchildmaybeabletoprovideimportantinformationrelatingtothehistoryoftheirsymptomsorthedegreeoffunctionaldifficultyexperienced.
Rheumaticdiseasesaresystemicdisorders,andthereforeacompletephysicalexaminationshouldbeperformedineverycase,duringwhichthechild'scomfort,modesty,anddignitymustberespected.Childrenshouldbeofferedappropriate-sizegownsorshorts,andshouldbegivenaprivatespaceforchangingclothes.Theapproachtothephysicalexaminationofthechildrequiresexpertiseinunderstandinghowtoapproachchildrenofdifferentages.Frequently,providinganexplanationtothechildofwhatwilloccurduringtheexaminationishelpful,andreassurancethattheexaminationwillnotcontinueifitcausespain.Inmostcases,examinationofpainfulareasshouldbelefttothelast.Forsmallchildren,theexaminationmaybeginbyobservingthechildatplayormovingaroundtheroom.Anapprehensiveyoungchildmayneedtohavethephysicalexaminationperformedwhilesittingonaparent'slap.Inmostcases,theskilledexaminerwillbeabletoperformacompleteexaminationofeventheyoungestchild.
Age-relatednormalvariationsinphysicalexaminationmustbetakenintoaccount:
Positionandrangeofmotion:Infull-termnewborns,theelbows,knees,andhipsdonotfullyextend.Intheyoungchild,oreventheadolescent,hyperextensionatthekneesandelbowsisoftengreaterthaninyearsofage.Asymmetryofrangeatanyageshouldbeconsideredabnormal.Manychildrenhaveflatfeetresultingfromthedistributionoffatandlimitedmuscledevelopmentuntiltheageof5or6years.Intheabsenceofsymptoms,noinvestigationortreatmentisrequired.Musclestrength:Evaluationofmusclestrengthintheyoungchildmaybedifficultduetodifficultyinthechild'sabilitytocooperateintheexaminationofindividualmusclegroups.Awelltrainedpaediatricphysiotherapistisoftenbestabletocompletelyassessachild'smusclestrengthreliably.Ambulation:Inordertobeabletoassessgaitinchildren,itiscriticaltoknowthenormaldevelopmentaltrajectoryofambulation(seeTable1.4).Childrenwhodeveloparthritisduringthetimetheyarelearningtowalkfrequentlypresentwithadelayinachievingambulation,regressioninmotormilestones,oranabnormalambulationpattern.Specificphysiotherapymayberequiredtocorrectpoorambulationhabitswhichpersistevenafteractivejointdiseaseiswell-controlled.Alimp(asymmetryofgait)mayresultfromstructuralasymmetry,pain,muscleweakness,orarthritis.Althoughitishelpfultodifferentiatebetweenapainfulandanon-painfullimp,itisimportanttonotethatsomechildrenwithactivearthritisinthelowerextremitymaynothavepain.Somecommoncausesoflimp,byageofthechild,arelistedinTable1.5.
-
The child patient
Page 10 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
Table1.5Commonorsignificantcausesoflimpingaccordingtoage
Toddler/preschoolInfection(septicarthritis,osteomyelitiship,spine)Mechanical(traumaandnon-accidentalinjury)Congenital/developmentalproblems(e.g.hipdysplasia,talipes)Neurologicaldisease(e.g.cerebralpalsy,hereditarysyndromes)JIAMalignantdisease(e.g.leukaemia,neuroblastoma)
510yearsMechanical(trauma,overuseinjuries,sportinjuries)Transientsynovitisirritablehip'LeggPerthesdiseaseJIATarsalcoalitionComplexregionalpainsyndromesMalignantdisease
1017yearsMechanical(trauma,overuseinjuries,sportinjuries)SlippedcapitalfemoralepiphysisJIAIdiopathicpainsyndromesOsteochonditisdissecansTarsalcoalitionComplexregionalpainsyndromesMalignantdisease(leukaemia,lymphoma,primarybonetumour)
JIA,juvenileidiopathicarthritis.
DiagnosisofchildhoodrheumaticdiseasesThechildwithmusculoskeletalpain
Manychildrenwithrheumaticdiseasewillpresenttothephysicianwithpain;however,itisimportanttonotethatnotallchildrenwithmusculoskeletalpainwillhavearheumaticdisease,andinfact,somechildrenwitharthritisandotherrheumaticconditionsdonothavepain.Therefore,theimportantjobofaphysicianevaluatingachildcomplainingofmusculoskeletalpainistoconsiderthebroaddifferentialdiagnosis,anduseclinicalcluesandphysicalexaminationtocometotheappropriatediagnosis.
Localizationofpaintothebone,joint,orsofttissuesmayhelpinguidingappropriateinvestigations,particularlyinthecontextoflengthoftimepainhasbeenpresent,severityofpain,orhistoryoftrauma.Veryseverepaininthecontextofanillchildwithfever,orthechild
24
-
The child patient
Page 11 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
whodoesnotallowmovementofajointorlimb,shouldbeinvestigatedforfracture,boneorjointinfection,ormalignancy.Jointpaininasingleormultiplejoints,moreprominentinthemornings,withgradualdifficultyinmovement,maybemoresuggestiveofarthritis.Painaftersportsactivitiesorexacerbatedbysportactivitiesmaybemechanicalororthopaedicinnature.
Paininyoungchildrenmaybeparticularlychallengingtoassess.Parentsmaynoteachildchangehowtheyusealimb,andonlywhenanareaisstressedorexaminedcarefullywillthechildcomplain.Someyoungchildrenmayrefusetouseanarmorleg,orregressinmotormilestonesasamanifestationofmusculoskeletalpain.Forexample,achildwhohasbeenwalkingbutstopswalking,limps,orholdsthefootinanabnormalpositionmayhavearthritisorotherproblems.Youngchildrenoftenlocalizepainpoorly,andthephysicianmustcarefullyidentifytheareaofdiscomfortbypalpationandobservationofthechild'sbehaviour.Thechildmaywithdrawthelimborbecomeanxiouswhentheaffectedareaisexamined.Someyoungchildrenareabletouseapainscaleutilizingfacestoscoretheirpain.
Painanddysfunctionmaybeasignofachronicidiopathicpainsyndrome,notarareconditioninadolescents.Theseadolescentspresentwitheitheraverylocalizedareaofpainandinabilitytousealimboradiffusepaininmanyareasofthebodyassociatedwithdisabilityandfatigue.Inpatientswithlocalizedpainsyndrome,anarthritiscannotbedemonstrated,andoftenabonescanmayshowdecreasedbloodflowtothearea;thisconditionissimilartoreflexsympatheticdystrophyandshouldbetreatedaggressivelywithphysiotherapy.Youngpeoplewithdiffusepainsyndromemayhavesofttissuetenderpointssimilartothoseseeninpatientswithfibromyalgia,aswellasfatigueandinabilitytoparticipateinnormalactivities.Thesepatientsmaybechallengingtotreat,astheyrequireamultidisciplinaryteamincludingphysiotherapy,occupationaltherapy,andpsychologyfortreatment.
Thechildwithbackpain
Backpainisanuncommoncomplaintinchildhood,particularlyinyoungchildren,ascomparedwithadults.Persistentcomplaintofbackpainshouldalwaysbethoroughlyinvestigated,astheunderlyingcausecouldbeseriousandrequireprompttreatment.Whenevaluatingachildwithbackpain,oneshouldconsiderthatbackpaincanbereferredfromotherareas;forexample,fromthebacktothethigh,fromthesacroiliacjointtothebuttock.ImportantcausesofbackpaininchildrenandadolescentsareshowninTable1.6.RedflagswhichshouldpromptclinicianconcernforseriousdiseaseareshowninTable1.7.
-
The child patient
Page 12 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
Table1.6Paininchildrenandadolescents
BackpainAcutetrauma
Fracture,dislocation,hematomaSpondylolysis,spondylolisthesis
TumourBenign(osteoidosteoma)Malignant(sarcoma,metastaticneuroblastoma,leukaemia,lymphoma)
InfectionDiscitisVertebralosteomyelitis
OsteoporosisScheurmann'sdiseaseDiffusepainsyndrome
PaininthesacroiliacjointsSepticsacroiliitisSpondyloarthropathy(arthritis)
PaininthepelvisOsteomyelitisChronicrecurrentmultifocalosteomyelitisTumour(usuallyosteogenicsarcomaorEwing'ssarcoma)
Table1.7Redflagsforevaluationofbackpaininchildrenandadolescents
Systemicfeatures:fever,nightsweat,weightlossNightpainNeurologicsymptomsorsignsGaitchangeChangeinbowelorbladderhabitsFocallowerextremitymuscleweaknessPainfulscoliosis
Thechildwithmonoarticulararthritis
Thedifferentialdiagnosisofmonoarticulararthritisinthechildoradolescentisbroad.Childrenwithanewpresentationofmonoarticulararthritisshouldbeevaluatedpromptly,becausepotentiallyseriouscausesmaynotpresentinthetypical'mannerseeninadults.SomeofthemorecommoncausesofmonoarticulararthritisinchildrenareshowninTable1.8.
-
The child patient
Page 13 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
Table1.8Monoarticulararthritisinchildrenandadolescents
Acutemonoarthritis Chronicmonoarthritis
InfectionSepticarthritis
InfectionOsteomyelitis
Osteomyelitis Chronicsepticarthritis(i.e.TB)
Trauma:minor,ligamentinjury,Fracture
JIA
Malignancy InflammatoryboweldiseaseOrthopaedic:osteochondritisdissecans,loosebodySynovialchondromatosisPigmentedvillonodularsynovitisOsteoidosteoma
JIA,juvenileidiopathicarthritis;TB,tuberculosis.
Thechildoradolescentwhopresentswithisolatedhippainoftenpresentsadiagnosticchallengefromseveralaspects.First,itiscriticaltoexamineallthejointsandaxialskeletoncarefully,withaviewtodifferentiatingthehippainfromthepossibilityofreferredpainfromotherareas.HippainasthesolepresentingfeatureofJIAisrelativelyrare,andthereforetheclinicianshouldconsiderthepossiblecausesofhippainaslistedinTable1.9.
-
The child patient
Page 14 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
Table1.9Causesofpersistenthippaininchildrenandadolescents
Condition Agerange/considerations
Congenitalhipdysplasia Usuallyfoundininfancybutcanbemissed
Transientsynovitis 310years
LeggPerthesdisease 510years;boysgirls
Slippedcapitalfemoralepiphysis 1015years;boysgirls
Idiopathicchondrolysisofthehip 1016years;girlsboys
Acutechondrolysisofthehip 1016years
JIAERA Anyage,usually8years
Reactivearthritis Anyage
Osteonecrosis Anyage
ERA,enthesitis-relatedarthritis;JIA,juvenileidiopathicarthritis.
Chronicasymmetricjointinflammationinthedevelopingchildcanresultinlocalizedgrowthdisturbances.Ingeneral,thebonesadjacenttoaninflamedjointgrowmorerapidly,andinconsequence,theaffecteddigitorlimbislonger.Ifthisoccursinasingleknee,ameasurableinequalityofthelegscanresult.Monitoringforlocalizedgrowthdisturbancesisanimportantpartoftheassessmentofachildwitharthritis,andmayindicateneedformoreaggressivetreatment.
Thechildwithmuscleweakness
Muscleweaknessiscommoninchildrenwithinflammatorymusculoskeletalconditions.SomechildrenwithJIAmaypresentwithapparentmuscleweaknessastheirmainsymptom,andonlyacompletephysicalexaminationwilldemonstratethefindingsofarthritis.Inaddition,anumberofrheumaticconditionspresentinchildhoodoradolescencewithweakness;theseincludejuveniledermatomyositis,mixedconnectivetissuedisease,andSLE.
Theevaluationofthechildwithmuscleweaknessmaybechallenging,particularlywhenthechildisyoung.Itmaybedifficulttodostandardmanualmuscletestinginayoungchild,becauseofthechild'sshortattentionspanordifficultyfollowinginstructions.Carefulobservationofthechildatplay,themannerinwhichtheygetupfromsittingorlyingorwalkintheexaminationroomorhallway,ortheirabilitytostandontiptoesandheels,orsquat,mayprovidethebestinformationaboutthechild'slevelofweakness.Forexample,thechildwithweaknessoftrunkandneckmuscles,asseenindermatomyositis,mayhavetorolloveron
-
The child patient
Page 15 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
theirsideorabdomentositfromasupineposition.ThechildwithweaknessofthehipgirdlemaybeunwillingtosquatorstandfromasquatwithoutshowingGower'ssign.Observationofthegaitforawide-basedorTrendelenburgsignmaysuggestweaknessofthehipgirdlemuscles.Assessmentofmusclestrengthshouldalsoincludeadetailedneurologicalexamination.Asymmetricweaknessisnotlikelytoresultfromaninflammatorymyositissuchasdermatomyositis,orfromaprimarymyopathy.Withpatienceandexperience,thephysicianorphysiotherapistcandemonstratemuscleweaknessbyformaltestinginthechildover34yearsofage.Theapplicationofastandardizedvalidmusclescoringscale,theChildhoodMyositisAssessmentScale,ishelpfulindeterminingthefunctionallevelofweakness,andtofollowchangesovertime.
Dermatomyositisissuggestedbythepresenceofsymmetricalproximalmuscleweakness;thepresenceoftheclassicalcutaneouschangesandelevatedserummuscleenzymeswillconfirmthediagnosisanddifferentiateitclinicallyfromprimarymyopathies.Weaknessofonelimbormusclemayindicateaperipheralneuropathiclesionorinflammationofanadjacentjointorjoints.Severeweaknessofthehipgirdleorthighscanresultfrominflammatorysacroilitisorgreatertrochantericenthesitis.
Thechildwithfeverofunknownorigin
Determiningthecauseoffeverofunknownorigin(FUO)inachildcanbechallenging,andfrequentlytheassistanceofapaediatricrheumatologistissought.Theconsultantmustfirstascertainthatthechildinfactdoeshavepersistentunexplainedfever,andthenmustthinkbroadlyacrossthedifferentialdiagnosis.Tobecertainthatthereisfever,actualdocumentationbyamedicalprofessional,sometimesinanin-patientsetting,mayberequired.Thisobservationperiodmaybehelpfulaswelltodeterminethefeverpattern,whichmaygiveacluetotheultimatediagnosis.
ThemostfrequentaetiologyofFUOisinfectious,andovertoroccultinfectionmustbesought.Abasicwork-upincludingcompletebloodcount,inflammatorymarkerssuchaserythrocytesedimentationrate(ESR)andC-reactiveprotein(CRP),liverandkidneyfunctiontesting,chestradiographs,andabdominalultrasoundmayberequired.Blood,urine,andotherbacterialculturesmustbeperformedtoruleoutoccultsepsisorbacterialendocarditis.Atechnetiumbonescanmaybeindicated.Itisalsoimportanttoconsiderandexcludemalignancyearlyinthework-upofachildwithFUO;thismayrequireabonemarrowbiopsy.Feverwithweightloss,thepresenceoferythemanodosum,arthritisorarthralgia,withorwithoutgastrointestinalsymptoms,maysuggestthepossibilityofinflammatoryboweldisease.Insuchinstances,theremaybeanaemia,hypoalbuminaemia,andelevationoftheESR.Definitivediagnosismayrequireendoscopyofthecolonorsmallbowelwithbiopsies;morerecently,MRIofthebowelhasbeenusedasadiagnostictest.
AmongtherheumaticconditionstobeconsideredinthechildwithFUOaresystemicarthritis,systemicvasculitis,SLE,orautoinflammatorysyndromes.
Theonsetofsystemicarthritismaybecharacterizedbyfeverandrashbeforethedevelopmentofjointdisease.Itisunusual,however,forarthritistolagmorethanafewweeksaftertheonsetofthesystemicfeaturesofthedisease;inaddition,adiagnosisofsystemicJIAintheabsenceofarthritisshouldbeconsideredtentative.Oneshouldbeaware,however,thatarthritismaypresentinsomewhatunusualpatterns:forexample,thechildwithneckpainand
-
The child patient
Page 16 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
torticollis,fever,andrashmayhavearthritisinthecervicalspineandthediagnosisofsystemicJIA.ThefeverofsystemicJIAisspecificallyquotidian,andtherashisevanescentandmacular;theadditionalpresenceofsystemicinflammatoryfeaturesofserositis,splenomegaly,anaemia,leucocytosis,andmarkedlyraisedESRarehelpfulmarkersofdisease.
Childrenwithvasculitismaypresentwithfeverandelevatedinflammatorymarkerswithoutobjectivephysicalsigns.InTakayasu'sarteritis,theremaybeaprolongedphaseofdiseasepriortodetectionofdeficienciesofperipheralpulses,makingdiagnosischallenging.Kawasaki'sdiseaseisusuallydiagnosedinchildrenearlyintheirfevercourse(withinthefirst10days);however,theremaybechildreninwhomthisdiagnosisismissed.Signsofrenaldisease,suchashypertensionorhaematuria,shouldbesoughtinchildrenwithFUO.Inpolyarteritis,thepresenceofpainfulsubcutaneousnodules,characteristicallyinthecalforsoleofthefoot,providestheopportunityforexcisionalbiopsy.
LaboratoryinvestigationsThelaboratoryevaluationofachildwithpresumedrheumaticdiseaseservesthreefunctions:toprovideorexcludeevidenceofinflammation,toprovidediagnosticevidence,andtoexcludenon-rheumaticdiseases.
Inscreeningforevidenceofinflammation,thewhitebloodcellcountanddifferential,haemoglobin,plateletcount,andESRorCRPgenerallysuffice.Somecluesfromthissimplebatteryoftestsmaybehelpful.AlowplateletcountinthepresenceofanelevatedESRshouldpromptconsiderationofanunderlyingmalignancy.InacuteKawasaki'sdisease,theplateletcountmayexceed10 ;childrenwithveryactivesystemiconsetJIAmayalsohaveextremeelevationsinplateletcounts.Decreasedserumalbumininachildwitharthritismaysuggestthepossibilityofinflammatoryboweldisease.
Teststhathavediagnosticspecificityforrheumaticdiseasesarefewinnumber.Althoughanti-nuclearantibody(ANA)ispresentinmanychildrenwithawidevarietyofrheumaticdiseases,itoccursinnon-rheumaticdiseaseandhealthychildrenaswell. Inthecontextofachildwitharthritisorothersymptomsstronglysuggestiveofarheumaticcondition,theantigenicspecificityoftheANAshouldbedeterminedandmaybehelpful.Antibodytodouble-strandedDNAorextractablenuclearantigenssuchasSSA/Ro,SSB/La,andSmarehighlysuggestiveofadiagnosisofSLE.AntibodiestocardiolipinandotherphospholipidantigenscanbeseeninpatientswithSLE,butcanbefoundinchildrenwithotherrheumaticandnon-rheumaticconditionsaswell.ElevatedlevelsofvonWillibrandfactorantigenoftenoccurinpatientswithinflammationofbloodvessels,suchasTakayasu'sarteritis,butalsoarefrequentlyelevatedinchildrenwithjuveniledermatomyositiswhendiseaseisactive.HighlyelevatedserumferritincanbeseeninchildrenwithactivesystemicJIA,andmaybeamarkerofhaemophagocyticsyndrome,apotentiallyfatalcomplicationofthisdisease.Antineutrophilcytoplasmicantibodies(ANCA)areusefulmarkersofvasculitidesinchildrensuchasgranulomatouspolyangiitis(formerlycalledWegener'sgranulomatosis),microscropicpolyangiitis,andpolyarteritisnodosa.
Thepresenceofarheumatoidfactor(RF)inachildwithmusculoskeletalpainisgenerallynothelpfulinmakingthediagnosisofarthritis.StudiesofthesensitivityandspecificityofRFinchildrenhaveshownthatithaslittlevalueasadiagnostictest.
6
25
26
-
The child patient
Page 17 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
Somelaboratoryinvestigationsareusefulinexcludingratherthandiagnosingdisease.Normalwhitebloodcellandplateletcounts,ESR,andCRPmakethepossibilityofarheumatic,malignant,orinfectiousdiseaselesslikely.Normalradiographsmaybehelpfulinexcludingsomeconditions;however,recent-onsetpathologycannotbeexcluded.Technetiumbonescanscanbeveryusefulinthissituation,andanormalthree-phasebonescanvirtuallyexcludesboneorjointdiseaseinachildwithundiagnosedmusculoskeletalpain.
References1.CassidyJT,PettyRE,LaxerRM,LindsleyCB.Textbookofpediatricrheumatology,6thedn.ElsevierSaunders,Philadelphia,PA,2011.
2.PettyRE,SouthwoodTR,MannersPJetal.InternationalLeagueofAssociationsforRheumatologyclassificationofjuvenileidiopathicarthritis:secondrevision,Edmonton,2001.JRheumatol2004;31(2):390392.
3.BrewerEJ,BassJ,BaumJetal.CurrentproposedrevisionoftheJRAcriteria.ArthritisRheum1977;20(Suppl):194199.
4.HoferM,SouthwoodTR.Classificationofchildhoodarthritis.BestPractResClinRheumatol2002;16(3):379396.
5.Special,WritingGroupoftheAmericanHeartAssociation.Guidelinesforthediagnosisofrheumaticfever.JAMA1992;268:20692073.
6.YellenES,GauvreauK,TakahashiMetal.Performanceof2004AmericanHeartAssociationrecommendationsfortreatmentofKawasakidisease.Pediatrics2010;125(2):e234e241.
7.HochbergMC.UpdatingtheAmericanCollegeofRheumatologyrevisedcriteriafortheclassificationofsystemiclupuserythematosus.ArthritisRheum1997;40:1725.
8.TanEM,CohenAS,FriesJFetal.The1982revisedcriteriafortheclassificationofsystemiclupuserythematosus.ArthritisRheum1982;25:12711277.
9.BohanA,PeterJB.Polymyositisanddermatomyositis.NewEnglJMed1975;292:344347.
10.FalkRJ,GrossWL,GuillevinLetal.Granulomatosiswithpolyangiitis(Wegener's):analternativenameofWegener'sgranulomatosis.ArthritisRheum2011;63(4):863864.
11.OzenS,PistorioA,IusanSMetal.EULAR/PRINTO/PREScriteriaforHenoch-Schonleinpurpura,childhoodpolyarteritisnodosa,childhoodWegenergranulomatosisandchildhoodTakayasuarteritis:Ankara2008.PartII:FinalClassificationcriteria.AnnRheumDis2010;69:798806.
12.HunderGG.Vasculitis:diagnosisandtreatment.AmJMed1996;100(supplA):3745.
13.RupertoN,OzenS,PistorioAetal.EULAR/PRINTO/PREScriteriaforHenoch-Schonleinpurpura,childhoodpolyarteritisnodosa,childhoodWegenergranulomatosisandchildhoodTakayasuarteritis:Ankara2008.PartI:Overallmethodologyandclinicalcharacterization.AnnRheumDis2010;69:790797.
-
The child patient
Page 18 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015
14.MannersPJ,BowerC.Worldwideprevalenceofjuvenilearthritis:whydoesitvarysomuch?JRheumatol2002;29(7):15201530.
15.MannersPJ,DiepeveenDA.Prevalenceofjuvenilechronicarthritisinapopulationof12yearoldchildreninurbanAustralia.Pediatrics1996;98:8490.
16.CassidyJ,PettyRE.Chronicarthritisinchildhood.In:CassidyJ,PettyRE,LaxerR,LindsleyCB(eds)Textbookofpediatricrheumatology,6thedn.ElsevierSaunders,Philadelphia,PA,2011:211235.
17.TuckerLB,DanceyP,OenKetal.;CanadianAllianceforPediatricRheumatologyInvestigators.Canadiannationalsurveillanceforjuvenileidiopathicarthritis.ArthritisRheum2008;suppl9.
18.TuckerLB,DanceyP,HuberA,OenK.Juvenileidiopathicarthritis:finalreport.CanadianPaediatricSurveillanceProgram,AnnualReport.http://web.www.cps.ca/English/surveillance/CPSP/Studies/2009Results.pdf2009;2629.
19.ChandrasekaranAN,RajendranCP,MadhavanR.JuvenilerheumatoidarthritisMadrasexperience.IndianJPediatr1996;63:501510.
20.SethV,KabraSK,SemwalOP,JainY.Clinico-immunologicalprofileinjuvenilerheumatoidarthritis-anIndianexperience.IndianJPediatr1996;63(3):293300.
21.TuckerLB,CabralDA.Transitionoftheadolescentpatientwithrheumaticdisease:issuestoconsider.RheumDisClinNorthAm2007;33(3):661672.
22.RobertsonL.Whenshouldyoungpeoplewithchronicrheumaticdiseasemovefrompaediatrictoadult-centeredcare?BestPractResClinRheumatol2006;20(2):387397.
23.MarshallB,TannerJM.Puberty.In:FalknerF,TannerJM(eds)Humangrowth:acomprehensivetreatise,2ndedn.Plenum,NewYork,1986:171209.
24.FosterH,TuckerLB.Musculoskeletaldisordersinchildrenandadolescents.In:AdebajoA(ed)ABCofrheumatology,4thedn.:BMJBooks,London,2009:98106.
25.CabralDA,PettyRE,FungM,MallesonPN.Persistentanti-nuclearantibodiesinchildrenwithoutidentifiableinflammatoryrheumaticorautoimmunedisease.Pediatrics1992;89(441):444.
26.EichenfieldAH,AthreyaB,DoughtyRA,CebulRD.Utilityofrheumatoidfactorinthediagnosisofjuvenilerheumatoidarthritis.Pediatrics1986;78:480484.
-
The child patient
Page 19 of 19
PRINTED FROM OXFORD MEDICINE ONLINE (www.oxfordmedicine.com). Oxford University Press, 2015. All RightsReserved. Under the terms of the l icence agreement, an individual user may print out a PDF of a single chapter of a title in OxfordMedicine Online for personal use (for details see Privacy Policy). Subscriber: Cristian Ninulescu; date: 16 July 2015