1 Keeping Pace with Targeted Therapies in Lung Cancer Highlights from the ASCO 2006 Annual Meeting.
-
date post
20-Dec-2015 -
Category
Documents
-
view
217 -
download
0
Transcript of 1 Keeping Pace with Targeted Therapies in Lung Cancer Highlights from the ASCO 2006 Annual Meeting.
1
Keeping Pace with Targeted Therapies in Lung CancerKeeping Pace with Targeted Therapies in Lung CancerHighlights from the ASCO 2006 Annual MeetingHighlights from the ASCO 2006 Annual Meeting
3
Overview of Targeted Therapies Overview of Targeted Therapies and Focus on Monoclonalsand Focus on Monoclonals
Karen Kelly, MDKaren Kelly, MDProfessor of MedicineProfessor of Medicine
Department of Medical OncologyDepartment of Medical OncologyUniversity of Colorado at DenverUniversity of Colorado at Denver
Aurora, ColoradoAurora, Colorado
4
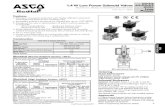
FDA-Approved Agents BeingFDA-Approved Agents BeingInvestigated for Lung Cancer TreatmentInvestigated for Lung Cancer Treatment
AgentAgent ClassClass TargetsTargets IndicationsIndications
Bevacizumab Bevacizumab (Avastin(Avastin®®; Genentech); Genentech)
Monoclonal (IV)Monoclonal (IV) VEGFVEGF CRCCRC
Cetuximab Cetuximab (Erbitux(Erbitux®®; ImClone); ImClone)
EGFREGFR Head & neck cancer, CRC Head & neck cancer, CRC
Erlotinib Erlotinib (Tarceva(Tarceva®®; Genentech); Genentech)
Reversible TKI (oral)Reversible TKI (oral) HER1/EGFRHER1/EGFR NSCLCNSCLC
Gefitinib Gefitinib (Iressa(Iressa®®; AstraZeneca); AstraZeneca)
HER1/EGFRHER1/EGFR NSCLCNSCLC
SunitinibSunitinib(Sutent(Sutent®®; Pfizer); Pfizer)
VEGFR-1, -2, -3; PDGFR-VEGFR-1, -2, -3; PDGFR-αα, -, -ββ; ; KIT; RET; FLT3KIT; RET; FLT3
RCC, GISTRCC, GIST
SorafenibSorafenib(Nexavar(Nexavar®®; Bayer); Bayer)
VEGFR-2, -3; cRAF; bRAF; VEGFR-2, -3; cRAF; bRAF; PDGFR-PDGFR-ββ; FLT3; KIT; FLT3; KIT
RCCRCC
BortezomibBortezomib(Velcade(Velcade®®, Millennium), Millennium)
Proteasome inhibitor Proteasome inhibitor (IV)(IV)
ProteasomeProteasome Multiple myelomaMultiple myeloma
Bexarotene Bexarotene (Targretin(Targretin®®; Ligand); Ligand)
Retinoid (oral)Retinoid (oral) RXRRXRαα, RXR, RXRββ, RXR, RXRγγ Cutaneous T-cell lymphomaCutaneous T-cell lymphoma
VEGF = vascular endothelial growth factor; CRC = colorectal cancer; EGFR = epidermal growth factor receptor; TK = tyrosine kinase; NSCLC = non–small-cell lung cancer; PDGFR = platelet-derived growth factor receptor; RCC = renal cell carcinoma; GIST = gastrointestinal stromal tumor;RXR = retinoid X receptor.
5
Examples of Novel Targeted Agents Being Examples of Novel Targeted Agents Being Investigated for Lung Cancer TreatmentInvestigated for Lung Cancer Treatment
Biologic TargetBiologic Target ClassClass Molecular TargetsMolecular Targets AgentAgent
TumorigenesisTumorigenesis Monoclonal Monoclonal (IV)(IV)
EGFREGFR Panitumumab Panitumumab (Amgen)(Amgen)
AngiogenesisAngiogenesis Reversible Reversible TKI (oral)TKI (oral)
VEGFR-1, -2, -3; VEGFR-1, -2, -3; PDGFR-PDGFR-ββ
VatalanibVatalanib(Novartis/Schering AG)(Novartis/Schering AG)
VEGFR-1, -2, -3; VEGFR-1, -2, -3; PDGFR; RETPDGFR; RET
AMG706 (Amgen)AMG706 (Amgen)
VEGFR-2VEGFR-2 AZD2171 (AstraZeneca)AZD2171 (AstraZeneca)
Angiogenesis + Angiogenesis + tumorigenesistumorigenesis
Dual Dual reversible TKI reversible TKI
(oral)(oral)
VEGFR-2, -3; RET; VEGFR-2, -3; RET; EGFREGFR
ZD6474 (Zactima; ZD6474 (Zactima; AstraZeneca)AstraZeneca)
TumorTumor Vaccine Vaccine (intradermal)(intradermal)
TGF-TGF-ββ antisense gene antisense gene modified allogeneic modified allogeneic tumor cell vaccinetumor cell vaccine
TGFTGFββAS Vaccine (Lucanix; AS Vaccine (Lucanix; NovaRx)NovaRx)
EGFR = epidermal growth factor receptor; TKI = tyrosine kinase inhibitor; VEGF = vascular endothelial growth factor; PDGFR = platelet-derived growth factor receptor; TGF = transforming growth factor.
6
ASCO 2006 UpdateASCO 2006 UpdateBevacizumab in NSCLCBevacizumab in NSCLC
Paclitaxel + carboplatin ± bevacizumab (updated Paclitaxel + carboplatin ± bevacizumab (updated results from randomized phase III trial E4599)results from randomized phase III trial E4599)
Sandler AB, et al.Sandler AB, et al.11
Brahmer JR, et al.Brahmer JR, et al.22
Dowlati A, et al.Dowlati A, et al.33
1. Sandler AB, et al. 41st ASCO; May 14-17, 2005. Abstract LBA4. 2. Brahmer JR, et al. 42nd ASCO;June 2-6, 2006. Abstract 7036. 3. Dowlati A, et al. 42nd ASCO; June 2-6, 2006. Abstract 7027.
7
Paclitaxel/Carboplatin ± Bevacizumab Paclitaxel/Carboplatin ± Bevacizumab Previously Reported ECOG 4599 ResultsPreviously Reported ECOG 4599 Results
Sandler AB, et al. 41st ASCO; May 14-17, 2005. Abstract LBA4.
PCPC(n = 427)(n = 427)
PCBPCB(n = 420)(n = 420) PP-Value-Value
Response rate, %*Response rate, %* 1010 27.227.2 < .0001< .0001
Median PFS, moMedian PFS, mo 4.54.5 6.46.4 < .0001< .00016-mo PFS, %6-mo PFS, % 32.632.6 55.055.0
1-y PFS, %1-y PFS, % 6.46.4 14.614.6
Median OS, moMedian OS, mo 10.210.2 12.512.5 .007.007
12-mo OS, %12-mo OS, % 43.743.7 51.951.9
24-mo OS, %24-mo OS, % 16.916.9 22.122.1*As percent of patients with measurable disease, n = 350 for the PC arm and n = 357 for PCB arm.ECOG = Eastern Cooperative Oncology Group; P = paclitaxel; C = carboplatin; B = bevacizumab;PFS = progression-free survival; OS = overall survival.
8
Paclitaxel/Carboplatin ± BevacizumabPaclitaxel/Carboplatin ± Bevacizumab Possible Gender Differences in Overall SurvivalPossible Gender Differences in Overall Survival
Unplanned subgroup analysis of ECOG 4599Unplanned subgroup analysis of ECOG 4599 Key finding: compared with males, females did not appear to gain Key finding: compared with males, females did not appear to gain
same overall survival benefit from addition of bevacizumabsame overall survival benefit from addition of bevacizumab
PCPC PCBPCB PP-Value-Value
Overall survival, moOverall survival, mo 10.3 10.3 12.312.3 .003.003Overall survival males, moOverall survival males, mo 8.78.7 11.711.7 .001.001
Overall survival females, moOverall survival females, mo 13.113.1 13.313.3 .87.87
Brahmer JR, et al. 42nd ASCO; June 2-6, 2006. Abstract 7036.
ECOG = Eastern Cooperative Oncology Group; P = paclitaxel; C = carboplatin; B = bevacizumab.
9
Paclitaxel/Carboplatin ± Bevacizumab Paclitaxel/Carboplatin ± Bevacizumab No Gender Differences in Overall SurvivalNo Gender Differences in Overall Survival
Females on PCB arm had higher response rate and progression-free Females on PCB arm had higher response rate and progression-free survival compared with females in the PC armsurvival compared with females in the PC arm
MalesMales FemalesFemales
PCPC(n = 230)(n = 230)
PCBPCB(n = 191)(n = 191) PP-Value-Value
PCPC(n = 162)(n = 162)
PCBPCB(n = 190)(n = 190) PP-Value-Value
Overall response Overall response rate (CR + PR), %rate (CR + PR), %
15.715.7 28.828.8 .001.001 14.214.2 41.141.1 < .0001< .0001
Progression-free Progression-free survival, mosurvival, mo
4.34.3 6.36.3 < .0001< .0001 5.35.3 6.26.2 .002.002
Brahmer JR, et al. 42nd ASCO; June 2-6, 2006. Abstract 7036.
P = paclitaxel; C = carboplatin; B = bevacizumab; CR = complete response; PR = partial response.
10
Paclitaxel/Carboplatin ± Bevacizumab Paclitaxel/Carboplatin ± Bevacizumab Perspective on Unplanned Analysis by GenderPerspective on Unplanned Analysis by Gender
Treatments at time of disease progression were not different, except that in Treatments at time of disease progression were not different, except that in the PCB arm, females were slightly less likely than males to get the PCB arm, females were slightly less likely than males to get chemotherapy as 2chemotherapy as 2ndnd-line therapy-line therapy
Reasons for observed differences in overall survival are unclear, possibilities Reasons for observed differences in overall survival are unclear, possibilities includeinclude– Random chanceRandom chance– Pitfalls of unplanned subgroup analysisPitfalls of unplanned subgroup analysis
These results contrast with results in CRC trials where no gender differences These results contrast with results in CRC trials where no gender differences reported in overall survivalreported in overall survival
PCB remains ECOG reference treatment in NSCLCPCB remains ECOG reference treatment in NSCLC
Brahmer JR, et al. 42nd ASCO; June 2-6, 2006. Abstract 7036.Laskin JJ. 42nd ASCO; June 2-6, 2006. Lung Cancer I Poster Discussion. Discussant.Hurwitz H, et al. Hurwitz H, et al. N Engl J MedN Engl J Med. 2004;350:2335.. 2004;350:2335.Genentech data on fileGenentech data on file
PCB = paclitaxel/carboplatin/bevacizumab; CRC = colorectal cancer; ECOG = Eastern Cooperative OncologyGroup; NSCLC = non–small-cell lung cancer.
11
Prospective Correlative Assessment of Prospective Correlative Assessment of Biomarkers from ECOG 4599Biomarkers from ECOG 4599
Biomarkers studiedBiomarkers studied Endothelial leukocyte adhesion molecule-1 (E-selectin)Endothelial leukocyte adhesion molecule-1 (E-selectin)
– Expressed only on endothelial cell after activation by inflammatory cytokinesExpressed only on endothelial cell after activation by inflammatory cytokines– Elevated E-selectin seen in disorders characterized by endothelial cell Elevated E-selectin seen in disorders characterized by endothelial cell
apoptosis and malignanciesapoptosis and malignancies Intercellular adhesion molecule-1 (ICAM-1; CD54)Intercellular adhesion molecule-1 (ICAM-1; CD54)
– Expressed on endothelial, epithelial, lymphocytes, monocytes, hepatocytes, Expressed on endothelial, epithelial, lymphocytes, monocytes, hepatocytes, and hemapoietic cellsand hemapoietic cells
– Elevated levels seen in many malignancies and alterations seen with Elevated levels seen in many malignancies and alterations seen with vascular targeting and antiangiogenic agentsvascular targeting and antiangiogenic agents
Vascular endothelial growth factor (VEGF) and basic-fibroblast growth factor (b-Vascular endothelial growth factor (VEGF) and basic-fibroblast growth factor (b-FGF)FGF)– Well-known angiogenic factorsWell-known angiogenic factors
Dowlati A, et al. 42nd ASCO; June 2-6, 2006. Abstract 7027.
12
Prospective Correlative Assessment of Prospective Correlative Assessment of Biomarkers From ECOG 4599—ResultsBiomarkers From ECOG 4599—Results
Dowlati A, et al. 42nd ASCO; June 2-6, 2006. Abstract 7027. Reprinted with permission from Dr. Dowlati.Hirsch F. 42nd ASCO; June 2-6, 2006. Lung Cancer III. Discussant.
Baseline plasma ICAM may be Baseline plasma ICAM may be prognostic for response and survival in prognostic for response and survival in advanced NSCLCadvanced NSCLC
– This might be useful stratification This might be useful stratification factor in future trialsfactor in future trials
– Low levels indicate a 2-fold Low levels indicate a 2-fold increase in likelihood of response increase in likelihood of response to chemotherapy (unclear if this is to chemotherapy (unclear if this is prognostic or predictive)prognostic or predictive)
Future trials are needed to determine Future trials are needed to determine if these will be better markers for if these will be better markers for clinical outcome than conventional clinical outcome than conventional radiographic response assessmentradiographic response assessment
Pro
bab
ility
Months
1.0 -
0.8 -
0.6 -
0.4 -
0.2 -
0.0 -
Survival by Baseline ICAMSurvival by Baseline ICAM
0 10 20 30 40
<260.5 (62 deaths/75 cases)>260.5 (70 deaths/75 cases)
P = .000050
1 y 60%
1 y 25%
13
Risk Factors for Pulmonary Hemorrhage (PH) Risk Factors for Pulmonary Hemorrhage (PH) in Bevacizumab-Treated Patientsin Bevacizumab-Treated Patients
Retrospective study of ECOG 4599 data examining association Retrospective study of ECOG 4599 data examining association between baseline clinical factors and incidence of early onset between baseline clinical factors and incidence of early onset (< 150 d from initial treatment) PH(< 150 d from initial treatment) PH Grade Grade 3 PH occurred in 2.3% of patients 3 PH occurred in 2.3% of patients Of 10 cases identified, 6 met criteria for early onset PH relatedOf 10 cases identified, 6 met criteria for early onset PH related
to bevacizumabto bevacizumab Pretreatment cavitation may be associated with increased riskPretreatment cavitation may be associated with increased risk
of PHof PH Hemoptysis was predicative of possible future PHHemoptysis was predicative of possible future PH
Sandler AB, et al. 42nd ASCO; June 2-6, 2006. Abstract 7068.
14
ASCO 2006 Update on ASCO 2006 Update on Cetuximab in NSCLCCetuximab in NSCLC
SWOG 0342 phase II trial of chemotherapy + SWOG 0342 phase II trial of chemotherapy + cetuximab vs chemotherapy followed by cetuximab vs chemotherapy followed by cetuximabcetuximab11
FLEX phase III trial of cisplatin/vinorelbine ± FLEX phase III trial of cisplatin/vinorelbine ± cetuximabcetuximab22
1. Kelly K, et al. 42nd ASCO; June 2-6, 2006. Abstract 7015.2. Von Pawl, J, et al. 42nd ASCO; June 2-6, 2006. Abstract 7109.
15
Preliminary Results of SWOG 0342 Phase II Preliminary Results of SWOG 0342 Phase II Trial of Paclitaxel/Carboplatin + CetuximabTrial of Paclitaxel/Carboplatin + Cetuximab
Primary objectives Primary objectives Compare response rate and toxicity of concurrent vs sequential Compare response rate and toxicity of concurrent vs sequential
platinum-based chemotherapy + cetuximab regimens as 1platinum-based chemotherapy + cetuximab regimens as 1stst-line-linetreatment for advanced NSCLCtreatment for advanced NSCLC
Select regimen for future trials based on overall survivalSelect regimen for future trials based on overall survival
Kelly K, et al. 42nd ASCO; June 2-6, 2006. Abstract 7015. Reprinted with permission from Dr. Kelly.
Randomize stage IIIB/IV
NSCLCPaclitaxel/carboplatin× 4 cycles(n = 119)
Paclitaxel/ carboplatin +
cetuximab× 4 cycles(n = 106)
Cetuximab weekly × 1
year
Cetuximab weekly × 1
year
16
Phase II Trial ofPhase II Trial ofPaclitaxel/Carboplatin + CetuximabPaclitaxel/Carboplatin + Cetuximab
Preliminary Efficacy ResultsPreliminary Efficacy Results
Kelly K, et al. 42nd ASCO; June 2-6, 2006. Abstract 7015.
Chemo Chemo Cetuximab Cetuximab (n = 119)*(n = 119)*
Chemo + Chemo + Cetuximab Cetuximab (n = 106)*(n = 106)*
Complete responseComplete response 00 00Partial response, % (95% CI)Partial response, % (95% CI) 25 (17–36)25 (17–36) 37 (26–49)37 (26–49)Stable disease, % (95% CI)Stable disease, % (95% CI) 44 (33–55)44 (33–55) 38 (27–50)38 (27–50)Disease stabilization, %Disease stabilization, %
(95% CI)(95% CI)69 (58–78)69 (58–78) 75 (63–84)75 (63–84)
Progression-free survival, moProgression-free survival, mo 44 44Median overall survival, moMedian overall survival, mo 99 10101-year overall survival, %1-year overall survival, % 4343 4949*Patients evaluable for response: 71 in the chemo + cetuximab arm and 87 in the chemo-only arm.
17
SWOG 0342—Phase II Trial of SWOG 0342—Phase II Trial of Paclitaxel/Carboplatin + CetuximabPaclitaxel/Carboplatin + Cetuximab
Preliminary Safety ResultsPreliminary Safety Results
Kelly K, et al. 42nd ASCO; June 2-6, 2006. Abstract 7015. Reprinted with permission from Dr. Kelly.
% o
f E
valu
able
Pat
ien
ts
Chemo +/- C
80 -
70 -
60 -
50 -
40 -
30 -
20 -
10 -
0 -
Adverse Events (grade 3/4)Adverse Events (grade 3/4)
Post-Chemo C
55
67
2027
N=101 N=94
N=20 N=22
Sequential
Concurrent
% o
f E
valu
able
Pat
ien
ts
Chemo +/- C
14 -
12 -
10 -
8 -
6 -
4 -
2 -
0 -
Rash (grade 3/4)Rash (grade 3/4)
Post-Chemo C
1
12
10N=94
N=20 N=22
No new cases concurrent ann
Sequential
Concurrent
Grade 3/4 AE (>5%) on Chemo (+/-C) Grade 3/4 AE (>5%) on Chemo (+/-C)
AdverseAdverse
EventEvent
Chemo + CChemo + C
N = 94N = 94
Chemo CChemo C
N = 94N = 94 P-P-ValueValue
DyspneaDyspnea 6.46.4 44 NSNS
FatigueFatigue 8.58.5 99 NSNS
LeukocytesLeukocytes 1616 18.818.8 NSNS
Joint painJoint pain 6.46.4 33 NSNS
NauseaNausea 6.46.4 22 NSNS
NeuropathyNeuropathy 1515 5.95.9 .04.04
NeutrophilsNeutrophils 41.441.4 36.636.6 NSNS
Chemo = paclitaxel/carboplatin; C = cetuximab.N=101
18
Phase II Trial ofPhase II Trial ofPaclitaxel/Carboplatin + CetuximabPaclitaxel/Carboplatin + Cetuximab
Preliminary ConclusionsPreliminary Conclusions
Concurrent cetuximab + chemotherapy arm met Concurrent cetuximab + chemotherapy arm met predetermined 10-month minimal median survival predetermined 10-month minimal median survival requirementrequirement
Trend toward higher response rate in concurrent armTrend toward higher response rate in concurrent arm Rash only significant additional toxicity seen with Rash only significant additional toxicity seen with
concurrent administration of cetuximab + chemotherapyconcurrent administration of cetuximab + chemotherapy Biomarker correlative studies ongoingBiomarker correlative studies ongoing New trials with this concurrent regimen + bevacizumab New trials with this concurrent regimen + bevacizumab
plannedplanned
Kelly K, et al. 42nd ASCO; June 2-6, 2006. Abstract 7015.
19
Phase III Trial ofPhase III Trial ofCisplatin/Vinorelbine ± CetuximabCisplatin/Vinorelbine ± Cetuximab
Preliminary Safety ReportPreliminary Safety Report Stage IIIB with documented malignant pleural effusion or stage IV Stage IIIB with documented malignant pleural effusion or stage IV
previously untreated NSCLCpreviously untreated NSCLC Epidermal growth factor receptor expression by Epidermal growth factor receptor expression by
immunohistochemistryimmunohistochemistry Patients recruited from 166 centers in 29 countries in Europe, Asia, Patients recruited from 166 centers in 29 countries in Europe, Asia,
Australia, and South AmericaAustralia, and South America Primary objective: overall survivalPrimary objective: overall survival Preplanned analysis by Data Safety Monitoring Board (DSMB) of Preplanned analysis by Data Safety Monitoring Board (DSMB) of
baseline and safety data from 365 patientsbaseline and safety data from 365 patients ResultsResults
– Recruitment completed in February 2006Recruitment completed in February 2006– 1125 patients randomized1125 patients randomized– Trial continuesTrial continues
Von Pawl J, et al. 42nd ASCO; June 2-6, 2006. Abstract 7109.
20
SWOG S0339—Phase II Trial of Bortezomib + SWOG S0339—Phase II Trial of Bortezomib + Gemcitabine/CarboplatinGemcitabine/Carboplatin
DesignDesign– Primary endpoint: OS (goal 10 month median OS to rule out Primary endpoint: OS (goal 10 month median OS to rule out
null hypothesis)null hypothesis)– Stage IIIB (with pleural effusion) or IV NSCLC, Stage IIIB (with pleural effusion) or IV NSCLC,
chemotherapy-naivechemotherapy-naive– PS = 0 or 1PS = 0 or 1
ResultsResults– N = 121 accrued (116 eligible)N = 121 accrued (116 eligible)– Median age: 64 years (range, 28–78)Median age: 64 years (range, 28–78)– 11% stage IIIB, 86% stage IV11% stage IIIB, 86% stage IV– Median follow-up: >15 monthsMedian follow-up: >15 months– Median number of cycles: 3.6Median number of cycles: 3.6
Davies AM, et al. 42nd ASCO; June 2-6, 2006. Abstract 7017.
SWOG = Southwest Oncology Group; OS = overall survival; PS = performance status.
21
Phase II Trial of BortezomibPhase II Trial of Bortezomib+ Gemcitabine/ Carboplatin+ Gemcitabine/ Carboplatin
Efficacy and Safety ResultsEfficacy and Safety Results
ResponseResponseNo. (%)No. (%)
(n = 114)(n = 114)
ORRORR 24 (21)24 (21)
CRCR 2 (2)2 (2)
PRPR 22 (19)22 (19)
SDSD 51 (45)51 (45)
PDPD 21 (18)21 (18)
Not evaluableNot evaluable 18 (16)18 (16)
Davies AM, et al. 42nd ASCO; June 2-6, 2006. Abstract 7017.
Overall survival 11 months (95% CI 8.2–13 months)Overall survival 11 months (95% CI 8.2–13 months) 1-year survival 47%; 2-year survival 14%1-year survival 47%; 2-year survival 14% Results above predetermined statistical endpoint to proceed to a phase III trialResults above predetermined statistical endpoint to proceed to a phase III trial
Grade 3/4 Toxicity inGrade 3/4 Toxicity in> 10% of Patients> 10% of Patients
No. (%)No. (%)(n = 114)(n = 114)
Neutropenia Neutropenia 59 (52)59 (52)
ThrombocytopeniaThrombocytopenia 72 (63)72 (63)
AnemiaAnemia 15 (13)15 (13)
FatigueFatigue 15 (13)15 (13)
AST/ALTAST/ALT 14 (12)14 (12)
ORR = overall response rate; CR = complete response; PR = partial response; SD = stable disease;PD = progressive disease; AST = aspartate aminotransferase; ALT = alanine aminotransferase.
22
SummarySummary
Clarification with regards to carboplatin/paclitaxel ± bevacizumab Clarification with regards to carboplatin/paclitaxel ± bevacizumab phase III trial ECOG 4599phase III trial ECOG 4599
–Bevacizumab does have some differential gender effectBevacizumab does have some differential gender effecton overall survival, but not clinically meaningfulon overall survival, but not clinically meaningful
–Potential predictive or prognostic biomarkersPotential predictive or prognostic biomarkers–Risk factors for bevacizumab-associated pulmonaryRisk factors for bevacizumab-associated pulmonary
hemorrhagehemorrhage Promising results from phase II trialsPromising results from phase II trials
–Cetuximab + carboplatin/paclitaxelCetuximab + carboplatin/paclitaxel–Cetuximab + cisplatin/vinorelbineCetuximab + cisplatin/vinorelbine–Bortezomib + gemcitabine/carboplatinBortezomib + gemcitabine/carboplatin
Data from phase III trials needed for cetuximab and bortezomibData from phase III trials needed for cetuximab and bortezomib
23
Focus on Small Molecules and Focus on Small Molecules and Investigational AgentsInvestigational Agents
Roy S. Herbst, MD, PhDRoy S. Herbst, MD, PhDProfessor of MedicineProfessor of Medicine
Department of Thoracic/Head Department of Thoracic/Head and Neck Medical Oncologyand Neck Medical Oncology
University of Texas University of Texas M.D. Anderson Cancer CenterM.D. Anderson Cancer Center
Houston, TexasHouston, Texas
24
Update on Small Molecule Update on Small Molecule and Investigational Agentsand Investigational Agents
Tyrosine kinase inhibitors Tyrosine kinase inhibitors with FDA approvalswith FDA approvals– SunitinibSunitinib– SorafenibSorafenib– ErlotinibErlotinib– GefitinibGefitinib
Investigational agentsInvestigational agents– VatalanibVatalanib– ZD6474ZD6474– ABI-007ABI-007– AMG706/panitumumabAMG706/panitumumab
BiomarkersBiomarkers– OsteopontinOsteopontin– EGF, Her2, p-AktEGF, Her2, p-Akt– RXR-beta, pPARyRXR-beta, pPARy
25
Tyrosine Kinase Inhibitors Target Both the Tumor and Endothelial CellsTyrosine Kinase Inhibitors Target Both the Tumor and Endothelial Cells
Endothelial Cell
VEGFR 1,2,3PDGFR
EGFRRAS-RAF
VEGFRNRP1
Tumor Cell
PDGF
VEGF
Endothelial Cell Pericytes
Nucleus Nucleus
VEGFR/PDGFRGrowth Factor Receptor
26
Similarities and Differences in Targets for TKIs Similarities and Differences in Targets for TKIs and Monoclonalsand Monoclonals
Tumor Endothelial cells
bFGFVEGFTGF-
Mechanism Inhibits tumor cell growth and blocks synthesis of angiogenetic proteins(eg, bFGF, VEGF, TGF-by tumor cells
Inhibits endothelial cells from responding to the angiogenic protein VEGF
Inhibitor Erlotinib Bevacizumab
Herbst RS, et al. J Clin Oncol. 2005;23:2544. Reprinted with permission from theAmerican Society of Clinical Oncology.
27
Sunitinib Phase II Trial in Previously Treated Sunitinib Phase II Trial in Previously Treated Advanced NSCLCAdvanced NSCLC
Open-label, single-arm, 2-stage multicenter trialOpen-label, single-arm, 2-stage multicenter trial Patients had recurrent stage IIIB/IV NSCLC that had failed 1 or more Patients had recurrent stage IIIB/IV NSCLC that had failed 1 or more
chemotherapy regimens (with/out EGFR inhibitor)chemotherapy regimens (with/out EGFR inhibitor) Sunitinib given at 50 mg/d for 4 wk followed by 2 wk off treatment before Sunitinib given at 50 mg/d for 4 wk followed by 2 wk off treatment before
next 6-week cyclenext 6-week cycle Primary endpoint: overall confirmed objective response rate (ORR)Primary endpoint: overall confirmed objective response rate (ORR) Enrollment Enrollment
– 63 patients63 patients– 64% had adenocarcinoma, 90% had stage IV disease64% had adenocarcinoma, 90% had stage IV disease– 43% had 1 prior regimen, 44% had 2 prior regimens, 13% had 3 or 43% had 1 prior regimen, 44% had 2 prior regimens, 13% had 3 or
more prior regimensmore prior regimens– 33% had received prior EGFR inhibitor33% had received prior EGFR inhibitor
Socinski MA et al. 42nd ASCO; June 2-6, 2006. Abstract 7001.
28
Sunitinib Phase II Trial inSunitinib Phase II Trial inPreviously Treated Advanced NSCLCPreviously Treated Advanced NSCLC
Safety ResultsSafety Results
Most toxicities were grade 1 or 2Most toxicities were grade 1 or 2 3 hemorrhage-related deaths on study: 2 (a pulmonary hemorrhage and 3 hemorrhage-related deaths on study: 2 (a pulmonary hemorrhage and
a cerebral hemorrhage) were considered study-drug relateda cerebral hemorrhage) were considered study-drug related
Socinski MA et al. 42nd ASCO; June 2-6, 2006. Abstract 7001.
Severe Events Occurring in Severe Events Occurring in 10% of Patients 10% of Patients % of Patients% of Patients
Adverse EventAdverse Event Grade 3Grade 3 Grade 4Grade 4
Fatigue/astheniaFatigue/asthenia 2222 55Pain/myalgiaPain/myalgia 1414 33Nausea/vomitingNausea/vomiting 1010 00DyspneaDyspnea 1313 00
29
Sunitinib Phase II Trial inSunitinib Phase II Trial inPreviously Treated Advanced NSCLCPreviously Treated Advanced NSCLC
Efficacy ResultsEfficacy Results
ResponseResponseNo. (%)No. (%)(n = 63)(n = 63)
ORRORR 6 (9.5)6 (9.5)95% CI (3.6–19.6)95% CI (3.6–19.6)
PRPR 6 (9.5)6 (9.5)
SDSD 27 (42.9)27 (42.9)
PDPD 14 (22.2)14 (22.2)
Not evaluableNot evaluable 16 (25.4)16 (25.4)
Best Response forBest Response forTarget Lesions by PatientTarget Lesions by Patient
100
80
60
40
20
0
-20
-40
-60
-80
-100
Cha
nge
from
Bas
elin
e (%
)
Partial Responses by RECIST
Stable Disease/Progressive Disease
Socinski MA et al. 42nd ASCO; June 2-6, 2006. Abstract 7001. Reprinted with permission from Dr. Socinski.
ORR = overall response rate; PR = partial response; SD = stable disease; PD = progressive disease;RECIST = response evaluation criteria in solid tumors.
Median duration of response: 12.2 weeks (range, 4.3–30.1+ weeks)Median duration of response: 12.2 weeks (range, 4.3–30.1+ weeks) Median PFS: 11.3 weeks (95% CI 10.0–15.7)Median PFS: 11.3 weeks (95% CI 10.0–15.7) Median OS: 23.9 weeks (95% CI 17.0–28.3)Median OS: 23.9 weeks (95% CI 17.0–28.3)
30
Phase II Trial of Sorafenib in Advanced NSCLCPhase II Trial of Sorafenib in Advanced NSCLC Primary objective: tumor response by RECIST of sorafenib 400 mg BID in Primary objective: tumor response by RECIST of sorafenib 400 mg BID in
previously treated ptspreviously treated pts EligibilityEligibility
– 1–2 prior treatments1–2 prior treatments– No prior gefitinibNo prior gefitinib– Asymptomatic brain metastases permittedAsymptomatic brain metastases permitted
EnrollmentEnrollment– 52 patients52 patients– Median age 62 years (range, 26–85)Median age 62 years (range, 26–85)– 85% ECOG PS = 185% ECOG PS = 1– 54% adenocarcinoma, 31% squamous cell carcinoma54% adenocarcinoma, 31% squamous cell carcinoma– 94% stage IV94% stage IV– 67% 1 prior chemotherapy; 29% 2 prior chemotherapy67% 1 prior chemotherapy; 29% 2 prior chemotherapy
Gatzemeier U, et al. 42nd ASCO; June 2-6, 2006. Abstract 7002.
RECIST = response evaluation criteria in solid tumors; ECOG = eastern cooperative oncology group;PS = performance status.
31
Phase II Trial of Sorafenib in Advanced NSCLCPhase II Trial of Sorafenib in Advanced NSCLCEfficacy ResultsEfficacy Results
ResponseResponse No. (%)No. (%)(n = 51)(n = 51)
SDSD 30 (59)30 (59)PDPD 18 (35)18 (35)Not evaluated*Not evaluated* 3 (6)3 (6)
60
40
20
0
-20
-40
-60
SD Patients PD Patients
Maximum Percentage Reduction of Maximum Percentage Reduction of Target Lesion by Patient (N = 48)Target Lesion by Patient (N = 48)††
*Patients died prior to tumor assessment. †48 patients with postbaseline tumor measurements available.Gatzemeier U, et al. 42nd ASCO; June 2-6, 2006. Abstract 7002. Reprinted with permission from Dr. Gatzemeier.
SD = stable disease; PD = progressive disease; PFS = progression-free survival; OS = overall survival.
Tumor cavitation in 4 patientsTumor cavitation in 4 patients Median PFS: 2.7 mo; median OS: 6.7 moMedian PFS: 2.7 mo; median OS: 6.7 mo SD patients: median PFS 5.5 moSD patients: median PFS 5.5 mo 2 patients treated for > 2 years with ongoing treatment2 patients treated for > 2 years with ongoing treatment
32
Phase II Trial of Sorafenib in Advanced NSCLCPhase II Trial of Sorafenib in Advanced NSCLCSafety and Biomarker Analysis ResultsSafety and Biomarker Analysis Results
SafetySafety– No grade 4 eventsNo grade 4 events– Grade 3 events: hand-foot skin Grade 3 events: hand-foot skin
reactions (20%), hypertension reactions (20%), hypertension (4%), diarrhea (2%), fatigue (2%), (4%), diarrhea (2%), fatigue (2%), headache (2%)headache (2%)
– 4 patients had sorafenib-related 4 patients had sorafenib-related bleeding events (3 epistaxis, 1 fatal bleeding events (3 epistaxis, 1 fatal pulmonary hemorrhage 30 days pulmonary hemorrhage 30 days after stopping sorafenib)after stopping sorafenib)
Biomarker analysisBiomarker analysis– Plasma biomarkers evaluated by Plasma biomarkers evaluated by
ELISAELISA– High VEGF at baseline High VEGF at baseline
correlated with shorter survival correlated with shorter survival ((PP < .05) < .05)
Su
rviv
al F
ract
ion
Time to Death (Days)
1.0
0.5
0.0
Low VEGFHigh VEGF
0 100 200 300 400 500 600 700
Gatzemeier U, et al. 42nd ASCO; June 2-6, 2006. Abstract 7002. Reprinted with permission from Dr. Gatzemeier.
ELISA = enzyme-linked immunosorbent assay; VEGF = vascular endothelial growth factor.
33
Phase II Trial of Sorafenib in Advanced NSCLC Phase II Trial of Sorafenib in Advanced NSCLC ConclusionsConclusions
Sorafenib has some activity in NSCLCSorafenib has some activity in NSCLC Historical comparisons show that 59% stable disease is in Historical comparisons show that 59% stable disease is in
same range as other targeted agents in NSCLCsame range as other targeted agents in NSCLC Agent generally well tolerated, with low incidence of bleedingAgent generally well tolerated, with low incidence of bleeding Deterioration of quality of life not seenDeterioration of quality of life not seen Shorter median overall survival correlated with high baseline Shorter median overall survival correlated with high baseline
VEGF and greater decreases in plasma VEGF during sorafenib VEGF and greater decreases in plasma VEGF during sorafenib treatmenttreatment
Phase III study of carboplatin/paclitaxel ± sorafenib is currently Phase III study of carboplatin/paclitaxel ± sorafenib is currently accruing patientsaccruing patients
Gatzemeier U, et al. 42nd ASCO; June 2-6, 2006. Abstract 7002.
34
Randomized Phase II Trial of Chemotherapy ± Randomized Phase II Trial of Chemotherapy ± Bevacizumab vs Erlotinib + Bevacizumab Bevacizumab vs Erlotinib + Bevacizumab
Phase II, multicenter 3-arm randomized trialPhase II, multicenter 3-arm randomized trial– Arm 1: chemotherapy (docetaxel or pemetrexed) + placeboArm 1: chemotherapy (docetaxel or pemetrexed) + placebo– Arm 2: chemotherapy (docetaxel or pemetrexed) + bevacizumabArm 2: chemotherapy (docetaxel or pemetrexed) + bevacizumab– Arm 3: erlotinib + bevacizumab Arm 3: erlotinib + bevacizumab
Arms 1 and 2 were double-blindedArms 1 and 2 were double-blinded Patients stratified by ECOG performance status and smoking historyPatients stratified by ECOG performance status and smoking history Eligibility: recurrent unresectable NSCLCEligibility: recurrent unresectable NSCLC Primary endpoint: safety and preliminary efficacyPrimary endpoint: safety and preliminary efficacy
Fehrenbacher L, et al. 42nd ASCO; June 2-6, 2006. Abstract 7062.
35
Phase II Chemotherapy ± Bevacizumab vs Phase II Chemotherapy ± Bevacizumab vs Erlotinib + BevacizumabErlotinib + Bevacizumab
EfficacyEfficacy
ChemotherapyChemotherapy
(n = 41)(n = 41)
Chemotherapy + Chemotherapy + BevacizumabBevacizumab
(n = 40)(n = 40)
Erlotinib + Erlotinib + BevacizumabBevacizumab
(n = 39) (n = 39)
Progression-free survivalProgression-free survival
Median, moMedian, mo 3.03.0 4.84.8 4.44.4
6-mo rate6-mo rate 21.5%21.5% 30.5%30.5% 33.6%33.6%
Adjusted HR* (95% CI)Adjusted HR* (95% CI) NANA 0.66 (0.38, 1.16)0.66 (0.38, 1.16) 0.72 (0.42,1.23)0.72 (0.42,1.23)
Unadjusted HR (95% CI)Unadjusted HR (95% CI) NANA 0.78 (0.47, 1.30)0.78 (0.47, 1.30) 0.76 (0.45, 1.28)0.76 (0.45, 1.28)
Overall survivalOverall survival
6-mo rate6-mo rate 62.4%62.4% 72.1%72.1% 78.3%78.3%
Response rateResponse rate
CR/PRCR/PR 12.2%12.2% 12.5%12.5% 17.9%17.9%
CR/PR/SDCR/PR/SD 39.0%39.0% 52.5%52.5% 51.3%51.3%
*Adjusted by randomization stratification factors (ECOG PS, smoking history).
Fehrenbacher L, et al. 42nd ASCO; June 2-6, 2006. Abstract 7062. Reprinted with permission from Dr. Fehrenbacher.
HR = hazard ratio; NA = not applicable; CR = complete response; PR = partial response; SD = stable disease.
36
Phase II Chemotherapy ± Bevacizumab vsPhase II Chemotherapy ± Bevacizumab vsErlotinib + BevacizumabErlotinib + Bevacizumab
SafetySafety
ToxicitiesToxicities
ChemotherapyChemotherapy(n = 41)(n = 41)
Chemotherapy + Chemotherapy + BevacizumabBevacizumab
(n = 40)(n = 40)
Erlotinib + Erlotinib + BevacizumabBevacizumab
(n = 39) (n = 39)
Most common overallMost common overall
FatigueFatigue 6666 7070 5656
NauseaNausea 4848 4242 4141
DiarrheaDiarrhea 1717 4040 6969
Rash/dermatitis/acneformRash/dermatitis/acneform 2929 2020 8282
AnemiaAnemia 2222 3232 1010
NeutropeniaNeutropenia 2424 3030 1010
Most common grade 3/4Most common grade 3/4
FatigueFatigue 1212 1212 77
NeutropeniaNeutropenia 1717 2020 55
Drug-related deathsDrug-related deaths 22 33 11
Fehrenbacher L, et al. 42nd ASCO; June 2-6, 2006. Abstract 7062. Reprinted with permission from Dr. Fehrenbacher.
Percent of PatientsPercent of Patients
37
Phase II Trial of Erlotinib vs Phase II Trial of Erlotinib vs Carboplatin/Paclitaxel in NSCLCCarboplatin/Paclitaxel in NSCLC
Primary endpoint: PFS (treatment worthy of further evaluation if PFS Primary endpoint: PFS (treatment worthy of further evaluation if PFS 3.5 3.5 months)months)
Study designStudy design– Eligibility: stage IIIB or IV no prior chemotherapyEligibility: stage IIIB or IV no prior chemotherapy– Performance status 2Performance status 2– No prior treatment with any EGFR inhibitor; no uncontrolled brain No prior treatment with any EGFR inhibitor; no uncontrolled brain
metastasesmetastases– Optional cross-over to erlotinibOptional cross-over to erlotinib
Enrollment: 103 patientsEnrollment: 103 patients Arms well balanced in demographics and baseline characteristicsArms well balanced in demographics and baseline characteristics
Lilenbaum R, et al. 42nd ASCO; June 2-6, 2006. Abstract 7022.
PFS = progression-free survival; EGFR = epidermal growth factor receptor.
38
Phase II Trial of Erlotinib vs Carboplatin/ Phase II Trial of Erlotinib vs Carboplatin/ Paclitaxel (CP) in NSCLCPaclitaxel (CP) in NSCLC
Efficacy ResultsEfficacy Results
No. of Pts (%)No. of Pts (%)
ResponseResponse ErlotinibErlotinib(n = 52)(n = 52)
CPCP(n = 51)(n = 51)
PRPR 1 (2)1 (2) 6 (12)6 (12)
SDSD 19 (37)19 (37) 21 (41)21 (41)
PDPD 23 (44)23 (44) 10 (20)10 (20)
Unable to Unable to determine/not determine/not evaluatedevaluated
8 (15)8 (15) 13 (25)13 (25)
Still on active Still on active therapytherapy
1 (2)1 (2) 1 (2)1 (2)
PF
S P
rob
abili
ty
PFS (Months)
1.0 -
0.9 -
0.8 -
0.7 -
0.6 -
0.5 -
0.4 -
0.3 -
0.2 -
0.1 -
0.0 -
Progression-Free Survival (PFS)Progression-Free Survival (PFS)
0 6 12 18 24 36
Group N Median(M) 95% ClErlotinib 52 1.91 (1.28, 2.69)PC 51 3.52 (1.48, 4.87)
Lilenbaum R, et al. 42nd ASCO; June 2-6, 2006. Abstract 7022. Reprinted with permission from Dr. Lilenbaum.
39
Phase II Trial of Erlotinib vsPhase II Trial of Erlotinib vsCarboplatin/Paclitaxel in NSCLCCarboplatin/Paclitaxel in NSCLC
ConclusionsConclusions
Single-agent erlotinib treatment did not meet progression-free Single-agent erlotinib treatment did not meet progression-free survival endpoint to warrant further evaluationsurvival endpoint to warrant further evaluation
Results in erlotinib-treated patients who developed grade 2+ Results in erlotinib-treated patients who developed grade 2+ rash were “in closer range to chemotherapy”rash were “in closer range to chemotherapy”
Sample size too small to make significant correlation between Sample size too small to make significant correlation between biomarkers analyzed and outcomebiomarkers analyzed and outcome
Quality of life parameters similar between 2 treatment armsQuality of life parameters similar between 2 treatment arms Development of erlotinib in 1st-line NSCLC centers onDevelopment of erlotinib in 1st-line NSCLC centers on
– Molecular selection of patientsMolecular selection of patients– Combination with other targeted agentsCombination with other targeted agents– Dosing optimizationDosing optimization
Lilenbaum R, et al. 42nd ASCO; June 2-6, 2006. Abstract 7022.
40
Molecular Predictors of Outcome with Erlotinib in Molecular Predictors of Outcome with Erlotinib in Bronchioloalveolar Cell Carcinoma (BAC)Bronchioloalveolar Cell Carcinoma (BAC)
Results of a prospective phase II trialResults of a prospective phase II trial Objective: compare clinical, pathologic, and molecular characteristics of tumor Objective: compare clinical, pathologic, and molecular characteristics of tumor
specimens associated with response, PFS, and OSspecimens associated with response, PFS, and OS Marker analysis: EGFR (mutations, amplification, polysomy, chromogenic in situ Marker analysis: EGFR (mutations, amplification, polysomy, chromogenic in situ
hybridization [CISH]), KRAS (mutations)hybridization [CISH]), KRAS (mutations)
Miller VA, et al. 42nd ASCO; June 2-6, 2006. Abstract 7003. Adapted with permission from Dr. Miller.
Outcome of Patients Treated with ErlotinibOutcome of Patients Treated with Erlotinib
n Median PFS Median OS(mo) (mo)
All 102 4 17
CR+PR 22 15 24Stable disease 38 6 29Progression 36 1 8Not evaluable 6 1 1
P < .01
Molecular Characteristics and OutcomeMolecular Characteristics and Outcome
Median PFS Median OSn RR(%) P (mo) P (mo) P
EGFR mut + 18 83 <.01 13 <.01 23 .65EGFR wt 64 7 2 17CISH ≥ 4 24 43 <.01 9 <.01 25 .38CISH < 4 53 13 2 16IHC ≥ 1 25 20 .99 4 .76 19 .60IHC 0 39 21 4 16KRAS mut + 19 0 <.01 4 .25 13 .24KRAS wt 62 32 5 21
41
Molecular Predictors of OutcomeMolecular Predictors of Outcomewith Erlotinib in BACwith Erlotinib in BAC
ConclusionsConclusions
Erlotinib resulted in 23% overall response rate (ORR) and 17 mo Erlotinib resulted in 23% overall response rate (ORR) and 17 mo median overall survival (OS) in BACmedian overall survival (OS) in BAC
Presence of EGFR mutation associated with an 83% ORR, Presence of EGFR mutation associated with an 83% ORR, 13 mo progression-free survival (PFS) and 22 mo OS13 mo progression-free survival (PFS) and 22 mo OS
EGFR amplification in BAC rareEGFR amplification in BAC rare EGFR polysomy predictive of improvement in PFSEGFR polysomy predictive of improvement in PFS KRAS exon 2 mutation associated with no responses and poorer OSKRAS exon 2 mutation associated with no responses and poorer OS Patients with EGFR mutation + CISH Patients with EGFR mutation + CISH 4 had ORR 90%, 4 had ORR 90%,
PFS 15 mo, OS 35 moPFS 15 mo, OS 35 mo Patients with wild type EGFR + CISH < 4 had ORR 4%, PFS 2 mo, Patients with wild type EGFR + CISH < 4 had ORR 4%, PFS 2 mo,
OS 15 moOS 15 mo
Miller VA, et al. 42nd ASCO; June 2-6, 2006. Abstract 7003.
42
Phase II Trial 1st-Line Erlotinib in PatientsPhase II Trial 1st-Line Erlotinib in Patientswith NSCLC and EGFR Mutationswith NSCLC and EGFR Mutations
Primary endpoint: time to progressionPrimary endpoint: time to progression EligibilityEligibility
– Stage IIIB/IV NSCLC + mutated EGFR Stage IIIB/IV NSCLC + mutated EGFR – No prior chemotherapyNo prior chemotherapy– No prior EGFR targeted agentsNo prior EGFR targeted agents
Paz-Ares L, et al. 42nd ASCO; June 2-6, 2006. Abstract 7020.
Response, % (95% CI)Response, % (95% CI) All (n = 38)All (n = 38) Exon 19 (n = 20)Exon 19 (n = 20) Exon 21 (n = 18)Exon 21 (n = 18)
ORRORR 82 82 (66–92)(66–92)
95 95 (75–100)(75–100)
67 67 (41–87)(41–87)
CRCR 13.213.2 2020 5.55.5
PRPR 68.468.4 7575 61.161.1
SDSD 13.213.2 55 22.222.2
PDPD 5.35.3 00 11.111.1
43
Phase II Trial 1st-Line Erlotinib in NSCLCPhase II Trial 1st-Line Erlotinib in NSCLCwith EGFR Mutationswith EGFR Mutations
ResultsResults
ConclusionsConclusions Most benefit: Exon 19 deletions, patients who never Most benefit: Exon 19 deletions, patients who never
smoked, visceral site other than lungsmoked, visceral site other than lung Phase III trial planned (erlotinib vs platinum-based Phase III trial planned (erlotinib vs platinum-based
chemotherapy in EGFR-mutated NSCLC)chemotherapy in EGFR-mutated NSCLC)
ORR P-value
EGFR Mutation .038
Exon 19 19 (95%)Exon 21 12 (67%)
Smoking .038Never 24 (90%)
Former 7 (70%)Current 0 (0%)
Gender .203
Female 22 (88%)Male 9 (69%)
ORR P-value
PS .662
0 8 (73%)1 18 (86%)2 5 (83%)
Histology .754
Adeno 23 (79%)BAC 4 (100%)
Other 4 (80%)
Stage 1.0
IIIB 4 (100%)IV 27 (79%)
Response PredictorsResponse Predictors
Paz-Ares L, et al. 42nd ASCO; June 2-6, 2006. Abstract 7020. Reprinted with permission from Dr. Paz-Ares.
TTP According to Smoking HabitsTTP According to Smoking Habits
TTP According to Mutational StatusTTP According to Mutational StatusLog Rank P =.06Breslow P =.06
Log Rank P =.12Breslow P =.02
44
Randomized Phase II Trial of ZD6474 vs Randomized Phase II Trial of ZD6474 vs Gefitinib in Advanced NSCLCGefitinib in Advanced NSCLC
Part A ResultsPart A Results
Secondary Efficacy Endpoint in Part ASecondary Efficacy Endpoint in Part A No. of Patients (%)No. of Patients (%)
ZD6474 (n = 83)ZD6474 (n = 83) Gefitinib (n = 85)Gefitinib (n = 85)
Objective responseObjective response 7 (8)7 (8) 1 (1)1 (1)
Disease control > 8 wkDisease control > 8 wk 37 (45)37 (45) 29 (34)29 (34)
Natale RB, et al. 42nd ASCO; June 2-6, 2006. Abstract 7000. Reprinted with permission from Dr. Natale.
Primary Endpoint in Part A:Primary Endpoint in Part A:Progression-Free SurvivalProgression-Free Survival
Individual Changes in Size of Target Individual Changes in Size of Target Lesions from Baseline: Part ALesions from Baseline: Part A
Pro
bab
ility
of
Rem
ain
ing
Pro
gre
ssio
n-F
ree
Progression-free survival in Part A (months)
Hazard ratio = 0.6995% Cl = 0.50 to 0.96Two-sided P-value = .025
Median PFS
ZD6474 = 11.0
Gefitinib = 8.1 weeks
Bes
t C
on
firm
ed
Ch
an
ge
fro
m B
as
eli
ne
in T
arg
et L
esi
on
Siz
e (
%)
ZD6474
Gefitinib
Final data cut-off, July 2005
45
Randomized Phase II Trial of ZD6474 vsRandomized Phase II Trial of ZD6474 vsGefitinib in Advanced NSCLCGefitinib in Advanced NSCLC
Part B ResultsPart B Results
Secondary Endpoint:Secondary Endpoint:Overall SurvivalOverall Survival
Median PFS
ZD6474 then gefitinib = 6.1 months
Gefitinib then ZD6474 = 7.4 months
Hazard ratio = 1.19(95% Cl = 0.84 to 1.68)Two-sided P-value = .34
Pro
ba
bil
ity
of
Re
ma
inin
g A
liv
e
Time to Death (months)Final data cut-off, July 2005
Natale RB, et al. 42nd ASCO; June 2-6, 2006. Abstract 7000. Reprinted with permission from Dr. Natale.
46
Randomized Phase II Trial of ZD6474 vs Gefitinib in Randomized Phase II Trial of ZD6474 vs Gefitinib in Advanced NSCLC: Adverse EventsAdvanced NSCLC: Adverse Events
Event*Event* ZD6474 (n = 83)ZD6474 (n = 83) Gefitinib (n = 85)Gefitinib (n = 85)
DiarrheaDiarrhea 58%58% 41%41%
Grade 3/4, no.Grade 3/4, no. 4/24/2 1/01/0
RashRash 46%46% 49%49%
Grade 3, no.Grade 3, no. 44 11
Nausea/vomitingNausea/vomiting 28%28% 34%34%
Grade 3, no.Grade 3, no. 11 11
HeadacheHeadache 18%18% 13%13%
Grade 3, no.Grade 3, no. 22 00
DizzinessDizziness 14%14% 9%9%
HypertensionHypertension 12%12% 1%1%
Grade 3, no.Grade 3, no. 33 00
QT-related eventsQT-related events 21%21% 5%5%
*AEs are all CTC grade 1 or 2 except where noted.Natale RB, et al. 42nd ASCO; June 2-6, 2006. Abstract 7000. Reprinted with permission from Dr. Natale.
47
Randomized Phase II Trial of ZD6474 vsRandomized Phase II Trial of ZD6474 vsGefitinib in Advanced NSCLCGefitinib in Advanced NSCLC
ConclusionsConclusions
Part A met primary endpoint of prolonging progression-free Part A met primary endpoint of prolonging progression-free survival (PFS)survival (PFS)– ZD6474 prolonged PFS by 45% compared with gefitinibZD6474 prolonged PFS by 45% compared with gefitinib
PFS prolongation did not result in overall survival PFS prolongation did not result in overall survival advantage in Part Badvantage in Part B– Why? Not clear, maybe optional switchover confounded Why? Not clear, maybe optional switchover confounded
survival assessmentsurvival assessment Adverse events (AEs) for both agents mostly mildAdverse events (AEs) for both agents mostly mild Slight differences in AE profilesSlight differences in AE profiles
Natale RB, et al. 42nd ASCO; June 2-6, 2006. Abstract 7000.
48
Novel Targeted Agents UnderNovel Targeted Agents UnderInvestigation for Lung Cancer TreatmentInvestigation for Lung Cancer Treatment
Highlights of ASCO 2006Highlights of ASCO 2006AgentAgent StudyStudy ResultsResults
AMG706AMG706 BlumenscheinBlumenscheinAbstract 7119Abstract 7119
Ongoing phase Ib trial in advanced NSCLC of AMG706 + CP, AMG706 + Ongoing phase Ib trial in advanced NSCLC of AMG706 + CP, AMG706 + panitumumab ± CPpanitumumab ± CP
TGFTGFββAS AS VaccineVaccine
NemunaitisNemunaitisAbstract 7018Abstract 7018
75 patients, safety of optimal dose determined, results suggest greater 75 patients, safety of optimal dose determined, results suggest greater survival compared with historical controls survival compared with historical controls
VatalanibVatalanib JahanJahanAbstract 7081Abstract 7081
Tolerated in mesotheliomaTolerated in mesotheliomaActivity: 8.5% PR, 68.1% SD Activity: 8.5% PR, 68.1% SD But 3-mo PFS (53.3%) did not met protocol-specified level of 75%But 3-mo PFS (53.3%) did not met protocol-specified level of 75%
ZD6474 ZD6474 Natale Natale Abstract 7000Abstract 7000
As shown in previous slides, ZD6474 produced longer PFS compared with As shown in previous slides, ZD6474 produced longer PFS compared with gefitinib in refractory NSCLCgefitinib in refractory NSCLC
HeymachHeymachAbstract 7016Abstract 7016
ZD6474 + docetaxel is being tested in ongoing double-blind, randomized ZD6474 + docetaxel is being tested in ongoing double-blind, randomized phase II trial in 2nd-line NSCLCphase II trial in 2nd-line NSCLC
ABI-007ABI-007 RizviRizviAbstract 7105Abstract 7105
Phase I/II trial, 1st-line in advanced NSCLC, MTD reached; ORR 30% and Phase I/II trial, 1st-line in advanced NSCLC, MTD reached; ORR 30% and 10.9 mo OS; grade 3 sensory neuropathy and fatigue, minimal 10.9 mo OS; grade 3 sensory neuropathy and fatigue, minimal myelosuppresion myelosuppresion
AZD2171AZD2171 LaurieLaurieAbstract 3054Abstract 3054
Phase I trial in advanced NSCLC of AZD2171 + CP; manageable toxicities Phase I trial in advanced NSCLC of AZD2171 + CP; manageable toxicities including hypertension; evidence of activityincluding hypertension; evidence of activity
CP = carboplatin/paclitaxel.
49
Other Searches for Useful Other Searches for Useful Biomarkers in NSCLC—ASCO 2006Biomarkers in NSCLC—ASCO 2006
Mack PC, et alMack PC, et al11
Elevated osteopontin plasma Elevated osteopontin plasma levels may have prognostic levels may have prognostic value in advanced NSCLCvalue in advanced NSCLC
Osteopontin is a secreted Osteopontin is a secreted glycoprotein involved in glycoprotein involved in induction of urokinase (uPA) induction of urokinase (uPA) and increased cell migrationand increased cell migration
Toschi L, et alToschi L, et al22
FISH or IHC analysis of samples FISH or IHC analysis of samples from 190 consecutive patients from 190 consecutive patients treated for advanced NSCLCtreated for advanced NSCLC
EGFR, HEr2, and p-Akt status are EGFR, HEr2, and p-Akt status are not predictors of sensitivity to not predictors of sensitivity to chemotherapychemotherapy
EGFR FISH + and/or HER2 EGFR FISH + and/or HER2 FISH+ patients seemed to benefit FISH+ patients seemed to benefit more from nonplatinum vs more from nonplatinum vs platinum-based combinations (but platinum-based combinations (but N small)N small)
In EGFR FISH+ patients, RR and In EGFR FISH+ patients, RR and TTP after EGFR-TKI used as 2nd-TTP after EGFR-TKI used as 2nd-line treatment were at least equal line treatment were at least equal to 1st-line chemotherapyto 1st-line chemotherapy
1. Mack PC, et al. 42nd ASCO, June 2-6, 2006. Abstract 7198.2. Toschi L, et al. 42nd ASCO, June 2-6, 2006. Abstract 7111.
50
SummarySummary
First-generation TKIs (gefitinib, erlotinib) the search continues forFirst-generation TKIs (gefitinib, erlotinib) the search continues for– Molecular markers for patient selectionMolecular markers for patient selection– Optimal combinationsOptimal combinations– Improved dosingImproved dosing
Multitargeted TKIs currently on the market (sorafenib, sunitinib)Multitargeted TKIs currently on the market (sorafenib, sunitinib)– Some promising, but not yet conclusive resultsSome promising, but not yet conclusive results
Investigational multitargeted TKIs (vatalanib, ZD6474, AMG706, AZ2171)Investigational multitargeted TKIs (vatalanib, ZD6474, AMG706, AZ2171)– Need data from randomized trialsNeed data from randomized trials– Some differences in adverse event profilesSome differences in adverse event profiles
General areas of needGeneral areas of need– Surrogate markers for evaluation of agentsSurrogate markers for evaluation of agents– Biomarkers for patient selectionBiomarkers for patient selection– Optimization of clinical trial designOptimization of clinical trial design
51
Toxicity Management of Targeted Toxicity Management of Targeted Therapies: Implications forTherapies: Implications forNursing and Managed CareNursing and Managed Care
Michelle Purdom, RN, BSNMichelle Purdom, RN, BSNManager, Clinical Trials OperationsManager, Clinical Trials Operations
Phase I ProgramPhase I ProgramUniversity of Texas University of Texas
M.D. Anderson Cancer CenterM.D. Anderson Cancer CenterHouston, TexasHouston, Texas
52
OverviewOverview
Management of side effects associated with Management of side effects associated with targeted therapiestargeted therapies
Pharmacoeconomics of cancer management Pharmacoeconomics of cancer management and role/implications of targeted therapies in and role/implications of targeted therapies in managed care settingmanaged care setting
53* Iressa was approved with contingencies on May 2, 2003.
Targeted Therapies and Approval DatesTargeted Therapies and Approval Dates
February 26, 2004
2003
May 2, 2003*
May 13, 2003
2004
February 12, 2004 November 19, 2004
2005
December 20, 2005
2006
January 26, 2006
QuickTime™ and aTIFF (LZW) decompressorare needed to see this picture.
54
Most Common Side Effects AssociatedMost Common Side Effects Associatedwith FDA-Approved Targeted Therapieswith FDA-Approved Targeted Therapies
Includes: *+IFL, +5-FU/LV, +FOLFOX4, and monotherapy; **+radiation, +irinotecan, and monotherapy; †+gemcitabine and monotherapy; ‡250 mg/d and 500 mg/d.
Side Effect Bevacizumab* Sunitinib Bortezomib Sorafenib Cetuximab** Erlotinib† Gefitinib‡
Abdominal pain Acne and/or rash Alopecia Altered taste Anemia Anorexia and/or weight loss Appetite decrease/ taste disorder Arthralgia/myalgia Asthenia Bleeding Constipation Cough Dehydration Diarrhea Dizziness Dry and/or discolored skin Dysesthesia and/or paresthesia Dyspepsia Dyspnea
55
Most Common Side Effects AssociatedMost Common Side Effects Associatedwith FDA-Approved Targeted Therapies with FDA-Approved Targeted Therapies (cont’d)(cont’d)
Includes: *+IFL, +5-FU/LV, +FOLFOX4, and monotherapy; **+radiation, +irinotecan, and monotherapy; †+gemcitabine and monotherapy; ‡250 mg/d and 500 mg/d.
Side Effect Bevacizumab* Sunitinib Bortezomib Sorafenib Cetuximab** Erlotinib† Gefitinib‡
Edema Epistaxis Fatigue Fever GI hemorrhage Hand-foot skin reaction Headache Hypertension Insomnia Leukopenia and/or neutropenia and/or thrombocytopenia Mucositis/stomatits Nausea and/or vomiting Pain Peripheral neuropathy Pharyngitis Proteinuria Pruritis Upper respiratory infection Xerostomia
56
Management of Bevacizumab-Associated Management of Bevacizumab-Associated Side EffectsSide Effects
Side EffectSide Effect ScopeScope Symptoms and ManagementSymptoms and Management
HypertensionHypertension Incidence Gr 3/4: B + C 12% vs C 2%Incidence Gr 3/4: B + C 12% vs C 2%Not infusion related; usually observed Not infusion related; usually observed during course of treatmentduring course of treatment
Standard oral antihypertensivesStandard oral antihypertensivesIf severe, temporarily suspend treatmentIf severe, temporarily suspend treatmentIf hypertensive crisis, discontinue treatmentIf hypertensive crisis, discontinue treatmentMonitor BP at least every 2–3 weeksMonitor BP at least every 2–3 weeks
AT eventsAT events Incidence B + C 4.4% vs C 1.9%Incidence B + C 4.4% vs C 1.9% Permanently discontinue treatmentPermanently discontinue treatment
GI perforationGI perforation Incidence: B + C 2–4% vs C 0.3%Incidence: B + C 2–4% vs C 0.3% Symptoms: abdominal pain, constipation, vomitingSymptoms: abdominal pain, constipation, vomiting
Wound healing or Wound healing or bleeding bleeding complicationscomplications
Incidence: among patients requiring surgery Incidence: among patients requiring surgery within 60 d of B + C 15% vs C 4%within 60 d of B + C 15% vs C 4%
Wait for complete healing of surgical incision and Wait for complete healing of surgical incision and at least 28 d after surgery before startingat least 28 d after surgery before startingB therapyB therapy
HemorrhageHemorrhage Incidence Gr 3–5 bleeding: B + C 5.2% vs Incidence Gr 3–5 bleeding: B + C 5.2% vs B 3.8% vs C 0.7%B 3.8% vs C 0.7%Incidence epistaxis (nosebleeds): B + C Incidence epistaxis (nosebleeds): B + C 35% vs C 10%35% vs C 10%
Epistaxis usually mild, use standard first aid Epistaxis usually mild, use standard first aid techniquestechniquesPatients with recent hemoptysis should not Patients with recent hemoptysis should not receive B therapyreceive B therapy
Sources: www.avastin.com/avastin/nurseFaqPro4.mAvastin (bevacizumab) prescribing information. Available at: http//www.gene.com/gene/products/information/oncology/avastin/insert.jsp
AT = arterial thromboembolic; B = bevacizumab; C = chemotherapy.
58
Management of Bortezomib-Associated Management of Bortezomib-Associated Side EffectsSide Effects
Side EffectSide Effect ScopeScope Symptoms and ManagementSymptoms and Management
Peripheral Peripheral neuropathyneuropathy
Incidence of new cases: 36% Incidence of new cases: 36% Gr 3, 7%Gr 3, 7%
Monitor patients for symptoms: burning sensation, hyperesthesia, Monitor patients for symptoms: burning sensation, hyperesthesia, hypoesthesia, paresthesia, discomfort, neuropathic painhypoesthesia, paresthesia, discomfort, neuropathic painNew and worsening neuropathy: depending on severity consider New and worsening neuropathy: depending on severity consider recommended changes in dose and schedulerecommended changes in dose and scheduleBefore initiating therapy, carefully consider risk/benefits of Before initiating therapy, carefully consider risk/benefits of bortezomib treatment for patients with pre-existing neuropathy bortezomib treatment for patients with pre-existing neuropathy
Asthenia Asthenia (fatigue, (fatigue, malaise, malaise, weakness)weakness)
Incidence: bortezomib 61% (Gr Incidence: bortezomib 61% (Gr 3/4, 12%) vs dexamethasone 3/4, 12%) vs dexamethasone 45% (Gr 3/4, 6%)45% (Gr 3/4, 6%)
Educate patients about caution in operating cars and other Educate patients about caution in operating cars and other machinery because of potential for fatigue, dizziness, syncope, machinery because of potential for fatigue, dizziness, syncope, hypotension, diplopia, blurred visionhypotension, diplopia, blurred visionEducate patients about avoiding dehydration and seeking medical Educate patients about avoiding dehydration and seeking medical advice if experience dizziness, light-headedness, or fainting spellsadvice if experience dizziness, light-headedness, or fainting spells
GI toxicitiesGI toxicities Incidence Gr 3 bortezomib 18% Incidence Gr 3 bortezomib 18% vs dexamethasone 6% (Gr 4 vs dexamethasone 6% (Gr 4 rare in both groups)rare in both groups)
Most common GI toxicities: nausea, diarrhea, constipation, Most common GI toxicities: nausea, diarrhea, constipation, vomiting, and anorexiavomiting, and anorexia
HypotensionHypotension Incidence: bortezomib 11% vs Incidence: bortezomib 11% vs dexamethasone 2%dexamethasone 2%
May need to adjust doses of antihypertensive medicationsMay need to adjust doses of antihypertensive medications
Velcade (bortezomib) prescribing information.
59
Management of Cetuximab-Associated Management of Cetuximab-Associated Side EffectsSide Effects
Side EffectSide Effect ScopeScope Symptoms and ManagementSymptoms and Management
Infusion reactionsInfusion reactions Incidence of severe Incidence of severe reactions: 2%–4%reactions: 2%–4%Incidence of Gr 1–2 Incidence of Gr 1–2 reactions: 16%–19%reactions: 16%–19%
Symptoms of severe (potentially fatal) reactions: rapid onset of airway Symptoms of severe (potentially fatal) reactions: rapid onset of airway obstruction (bronchospasm, stridor, hoarseness), urticaria, obstruction (bronchospasm, stridor, hoarseness), urticaria, hypertension, and/or cardiac arresthypertension, and/or cardiac arrestSymptoms of Gr 1–2 reactions: chills, fever, dyspnea on 1Symptoms of Gr 1–2 reactions: chills, fever, dyspnea on 1stst day of day of initial dosinginitial dosingSevere reactions: immediate and permanent cetuximab treatment Severe reactions: immediate and permanent cetuximab treatment discontinuationdiscontinuationMild/moderate reactions: slow infusion rate, use antihistamines (eg, Mild/moderate reactions: slow infusion rate, use antihistamines (eg, diphenhydramine) in subsequent dosesdiphenhydramine) in subsequent doses
Cardiopulmonary Cardiopulmonary arrestarrest
Incidence of arrest Incidence of arrest and/or sudden death: and/or sudden death: cetuximab + radiation cetuximab + radiation therapy 2% vs 0% for therapy 2% vs 0% for radiation therapyradiation therapy
Use with caution in patients with coronary heart disease, congestive Use with caution in patients with coronary heart disease, congestive heart failure, and arrhythmiasheart failure, and arrhythmiasClosely monitor serum electrolytes (including magnesium, potassium, Closely monitor serum electrolytes (including magnesium, potassium, calcium) during and after cetuximab therapycalcium) during and after cetuximab therapy
Dermatologic Dermatologic toxicitytoxicity
Incidence in CRC: 89% Incidence in CRC: 89% of all treated patients, of all treated patients, severe in 11%severe in 11%
Signs: acneform rash, skin drying and fissuringSigns: acneform rash, skin drying and fissuringMonitor for development of inflammatory and infectious sequelae; Monitor for development of inflammatory and infectious sequelae; consider topical and/or oral antibioticsconsider topical and/or oral antibioticsSevere acneform rash: institute dose modificationsSevere acneform rash: institute dose modificationsTopical corticosteroids not recommendedTopical corticosteroids not recommended
www.erbitux.com
60
Management of Erlotinib-Associated Management of Erlotinib-Associated Side EffectsSide Effects
Side EffectSide Effect ScopeScope Symptoms and ManagementSymptoms and Management
RashRash Overall incidence of rash: erlotinib Overall incidence of rash: erlotinib 75% vs placebo 17%75% vs placebo 17%Incidence of Gr 3 rash with erlotinib: Incidence of Gr 3 rash with erlotinib: 8%8%
Take erlotinib at the same time each day between Take erlotinib at the same time each day between meals (one hour before or two hours after eating).meals (one hour before or two hours after eating).Pts with severe skin reactions may need dose Pts with severe skin reactions may need dose reductions or interruptionsreductions or interruptions
DiarrheaDiarrhea Incidence of severe diarrhea: 6%Incidence of severe diarrhea: 6% Educate patients to seek prompt medical attention Educate patients to seek prompt medical attention for severe or persistent diarrheafor severe or persistent diarrheaUsually managed with loperamideUsually managed with loperamideUse dose reductions or interruptions in patients Use dose reductions or interruptions in patients who are dehydrated or have unresponsive severe who are dehydrated or have unresponsive severe diarrheadiarrhea
Interstitial Interstitial lung disease lung disease (ILD)(ILD)
Overall incidence of ILD-like events: Overall incidence of ILD-like events: 0.7%0.7%Most cases in lung cancer patients Most cases in lung cancer patients associated with confounding factorsassociated with confounding factors
Interrupt treatment for acute onset or progression Interrupt treatment for acute onset or progression of unexplained pulmonary symptomsof unexplained pulmonary symptomsIf ILD confirmed, discontinue treatmentIf ILD confirmed, discontinue treatmentEducate patients to seek prompt medical attention Educate patients to seek prompt medical attention for onset or worsening of unexplained shortness of for onset or worsening of unexplained shortness of breath or coughbreath or cough
www.tarceva.com.
61
Management of Gefitinib-Associated Management of Gefitinib-Associated Side EffectsSide Effects
Side EffectSide Effect ScopeScope Symptoms and ManagementSymptoms and Management
Interstitial lung Interstitial lung disease (ILD)disease (ILD)
Overall incidence: 1% of Overall incidence: 1% of gefitinib-treated patients (1/3 gefitinib-treated patients (1/3 of these cases were fatal)of these cases were fatal)
Symptoms: acute onset of dyspnea, sometimes Symptoms: acute onset of dyspnea, sometimes with cough or low-grade fever, often quickly with cough or low-grade fever, often quickly worsening and requiring hospitalizationworsening and requiring hospitalizationInterrupt treatment in patients with acute onset or Interrupt treatment in patients with acute onset or worsening of pulmonary symptoms (dyspnea, worsening of pulmonary symptoms (dyspnea, cough, fever)cough, fever)Discontinue gefitinib treatment if ILD confirmedDiscontinue gefitinib treatment if ILD confirmed
Eye toxicityEye toxicity Low incidence of eye pain and Low incidence of eye pain and corneal erosion/ulcer, corneal erosion/ulcer, sometimes with aberrant sometimes with aberrant eyelash growtheyelash growth
Consider therapy interruption until symptoms Consider therapy interruption until symptoms resolved and removal of aberrant eyelash (if resolved and removal of aberrant eyelash (if present)present)
www.iressa.com
Most common gefitinib-associated adverse events: diarrhea, rash, acne, dry skin, nausea, vomitingMost common gefitinib-associated adverse events: diarrhea, rash, acne, dry skin, nausea, vomiting
62
Example ofExample ofTypical Typical
Rash Induced by Rash Induced by EGFR InhibitorsEGFR Inhibitors
Courtesy of Michelle Purdom, RN, BSN
64
Management of Sunitinib-Associated Management of Sunitinib-Associated Side EffectsSide Effects
Side EffectSide Effect ScopeScope Symptoms and ManagementSymptoms and Management
GI eventsGI events Most common: diarrhea, nausea, Most common: diarrhea, nausea, stomatitis, dyspepsia, vomitingstomatitis, dyspepsia, vomiting
Supportive care with antiemetic or antidiarrhea medicationsSupportive care with antiemetic or antidiarrhea medications
Left ventricular Left ventricular dysfunctiondysfunction
Incidence: sunitinib 11% vs placebo 3%Incidence: sunitinib 11% vs placebo 3% Some patients recovered without interventionSome patients recovered without interventionPossible interventions: dose reduction, use of antihypertensive or Possible interventions: dose reduction, use of antihypertensive or diureticdiureticCarefully monitor patients for signs and symptoms of congestive Carefully monitor patients for signs and symptoms of congestive heart failureheart failure
HemorrhageHemorrhage Incidence of bleeding: sunitinib 18% vs Incidence of bleeding: sunitinib 18% vs placebo 17%placebo 17%Fatal pulmonary hemorrhage occurred in 2 Fatal pulmonary hemorrhage occurred in 2 patients in a sunitinib NSCLC clinical trialpatients in a sunitinib NSCLC clinical trial
Epistaxis most common hemorrhagic adverse eventEpistaxis most common hemorrhagic adverse event
HypertensionHypertension Incidence: sunitinib 15% (Gr 3, 4%) vs Incidence: sunitinib 15% (Gr 3, 4%) vs placebo 11% (Gr 3, 0)placebo 11% (Gr 3, 0)No Gr 4No Gr 4
Monitor and treat with standard hypertensiveMonitor and treat with standard hypertensiveIf severe, suspend sunitinib treatment until hypertension is If severe, suspend sunitinib treatment until hypertension is controlledcontrolled
Skin toxicitySkin toxicity Skin discoloration: occurs in 1/3 of ptsSkin discoloration: occurs in 1/3 of ptsAttributed to yellow drug colorAttributed to yellow drug color
Advise patients of potential occurrenceAdvise patients of potential occurrenceOther possible dermatologic effects: dryness, thickness or cracking Other possible dermatologic effects: dryness, thickness or cracking of skin, blister or rash on palms of hand and soles of feetof skin, blister or rash on palms of hand and soles of feet
www.sutent.com
65
Management of Sorafenib-Associated Management of Sorafenib-Associated Side EffectsSide Effects
Side EffectSide Effect ScopeScope Symptoms and ManagementSymptoms and Management
DermatologicDermatologic Hand-foot skin reaction (35%) Hand-foot skin reaction (35%) and rash (38%) most common and rash (38%) most common adverse eventadverse eventUsually Gr 1-2, appear during Usually Gr 1-2, appear during 11stst 6 weeks of treatment 6 weeks of treatment
Topical therapies for symptomatic reliefTopical therapies for symptomatic reliefTemporary treatment interruption or dose Temporary treatment interruption or dose modificationsmodificationsSevere or persistent cases may require treatment Severe or persistent cases may require treatment discontinuationdiscontinuation
HypertensionHypertension Incidence: sorafenib 16.9% vs Incidence: sorafenib 16.9% vs placebo 1.8%placebo 1.8%Usually mild to moderate and Usually mild to moderate and occurs early in treatmentoccurs early in treatment
BP should be monitored weekly for 1BP should be monitored weekly for 1stst 6 weeks of 6 weeks of sorafenib therapysorafenib therapyManage with standard antihypertensive therapyManage with standard antihypertensive therapyTemporary treatment interruption or dose Temporary treatment interruption or dose modificationsmodificationsTreatment discontinuation rareTreatment discontinuation rare
HemorrhageHemorrhage Incidence: sorafenib 15.3%Incidence: sorafenib 15.3%(Gr 3, 2%; no Gr 4) vs placebo (Gr 3, 2%; no Gr 4) vs placebo 8.2% (Gr 3, 1.3%; Gr 4 0.2%)8.2% (Gr 3, 1.3%; Gr 4 0.2%)
If bleeding necessitates medical intervention, If bleeding necessitates medical intervention, consider permanently discontinuing sorafenibconsider permanently discontinuing sorafenib
Cardiac ischemia Cardiac ischemia and/or infarctionand/or infarction
Incidence: sorafenib 2.9% vs Incidence: sorafenib 2.9% vs placebo 0.4%placebo 0.4%
Consider temporary or permanent treatment Consider temporary or permanent treatment discontinuation discontinuation
www. nexavar.com
66
Pharmacoeconomics of Cancer Pharmacoeconomics of Cancer Management and Role/Implications of Management and Role/Implications of
Targeted Therapies inTargeted Therapies inManaged Care SettingManaged Care Setting
Cohen M, et al. Am J Manag Care. 2006;12:524.
67
Targeted Therapies and Managed CareTargeted Therapies and Managed Care
New therapies need evidence of effectiveness New therapies need evidence of effectiveness and safetyand safety
Impact on quality of lifeImpact on quality of life Net impact on total cost of careNet impact on total cost of care Concept of value differs among patients, Concept of value differs among patients,
providers, health plans, and employersproviders, health plans, and employers
Cohen M, et al. Am J Manag Care. 2006;12:524.
68
Biotechnology PipelineBiotechnology Pipeline
AIDS/HIV infections/related conditionsAutoimmune disorders
Blood disordersCancer/related conditions
Cardiovascular diseaseEye conditions
Diabetes/related conditionsDigestive disorders
Genetic disordersGrowth disorder
Infectious diseaseNeurologic disorders
Other conditions not specified hereRespiratory disorders
Skin disordersTransplantation
2004 Survey. Medicines in Development: Biotechnology. Available at: http://www.phrma.org/files/Biotech%20survey.pdf. Accessed February 15, 2006.
1726
2154
1951011
93
431617
1473
Condition Number of Agents
69
Growth Drivers for BiologicsGrowth Drivers for Biologics
Key contributors from managed care perspective includeKey contributors from managed care perspective include Increased availability of targets for biologic agentsIncreased availability of targets for biologic agents Increased use of approved drugsIncreased use of approved drugs Increased approval of biotechnology drugs for more Increased approval of biotechnology drugs for more
common conditionscommon conditions Expanded indications for approved drugsExpanded indications for approved drugs
Cohen M, et al. Am J Manag Care. 2006;12:524-537. Reprinted with permission.
70
Reasons for Off-Label Use of BiologicsReasons for Off-Label Use of Biologics
Small population size and/or assessed cost of clinical trials may Small population size and/or assessed cost of clinical trials may discourage marketers from seeking formal FDA approvaldiscourage marketers from seeking formal FDA approval
Potential of newer therapies for better efficacy and outcomesPotential of newer therapies for better efficacy and outcomes Proven safety and efficacy in other disease statesProven safety and efficacy in other disease states Potential for increased quality of lifePotential for increased quality of life Thought leader advocacy/patient demandThought leader advocacy/patient demand Better understanding of disease pathways, particularly immune-Better understanding of disease pathways, particularly immune-
modulating diseasesmodulating diseases
Cohen M, et al. Am J Manag Care. 2006;12:524-537. Reprinted with permission.
71
Managed Care’s Concerns RegardingManaged Care’s Concerns RegardingOff-Label Use of BiologicsOff-Label Use of Biologics
Safety/efficacy questionsSafety/efficacy questions Differing dosing and administrationDiffering dosing and administration Potential for inappropriate carePotential for inappropriate care Potential for cost increasePotential for cost increase Paucity of dataPaucity of data Lack of uniform guidelines/best Lack of uniform guidelines/best
practicespractices Legal/ethical issuesLegal/ethical issues
Cohen M, et al. Am J Manag Care. 2006;12:524-537. Reprinted with permission.
72
Recommendations for Managing Recommendations for Managing Expanded IndicationsExpanded Indications
Scan the pipeline to become aware of impending drug Scan the pipeline to become aware of impending drug launcheslaunches
Increase education for P&T committeesIncrease education for P&T committees Define a process and clear criteriaDefine a process and clear criteria Develop and/or augment treatment guidelines for Develop and/or augment treatment guidelines for
expanded indicationsexpanded indications Increase case management/disease managementIncrease case management/disease management Strive for innovative management strategies that Strive for innovative management strategies that
contain cost and maintain accesscontain cost and maintain access
Cohen M, et al. Am J Manag Care. 2006;12:524.
73
Continued Challenges for Continued Challenges for Managed Care OrganizationsManaged Care Organizations
Expanding indications for FDA-approved drugs present uniqueExpanding indications for FDA-approved drugs present uniquechallenges for MCOs.challenges for MCOs.– This translates into added expenditures for MCOs because of increased This translates into added expenditures for MCOs because of increased
frequency of administration and/or longer duration of therapyfrequency of administration and/or longer duration of therapy– For patients, may result in higher copays and more restrictive access For patients, may result in higher copays and more restrictive access
management strategies, particularly the use of prior authorizationmanagement strategies, particularly the use of prior authorization Maintain focus on potential of agents for reduction in disease progression and Maintain focus on potential of agents for reduction in disease progression and
disability rather than solely on patient copays and aggressive management disability rather than solely on patient copays and aggressive management strategiesstrategies– Shift focus on cost to clinical decision making through evidence-based medicineShift focus on cost to clinical decision making through evidence-based medicine
Adequately plan for agents with multiple indicationsAdequately plan for agents with multiple indications– Need more definitive criteria for evaluating expanded indications and potential Need more definitive criteria for evaluating expanded indications and potential
for cost savingsfor cost savings
Cohen M, et al. Am J Manag Care. 2006;12:524.
74
Nursing ImplicationsNursing Implications
The nurse should help the patient understand The nurse should help the patient understand importance of prior insurance authorization due importance of prior insurance authorization due to the high cost of biopharmaceuticalsto the high cost of biopharmaceuticals
The nurse should assist the patient as a liaison The nurse should assist the patient as a liaison with the hospital business office/MCO by with the hospital business office/MCO by initiating the process early and ofteninitiating the process early and often
Emotional support Emotional support
75
SummarySummary
Expanding indications and off-label applications of FDA-approved Expanding indications and off-label applications of FDA-approved targeted therapies present unique challengestargeted therapies present unique challenges– MCOs face added expensesMCOs face added expenses– Patients face higher co-pays and more restrictive access Patients face higher co-pays and more restrictive access – Clinicians need to expand their knowledge base and skill setsClinicians need to expand their knowledge base and skill sets
Nurses have an important role in providing Nurses have an important role in providing – Professional careProfessional care– Toxicity management and side effect educationToxicity management and side effect education– Assistance in navigating the preauthorization processAssistance in navigating the preauthorization process– Emotional supportEmotional support