1 HEMOSTASIS Is a complex of homeostatic reactions, which result in arrest of bleeding from damaged...
-
Upload
oswald-owen -
Category
Documents
-
view
215 -
download
0
Transcript of 1 HEMOSTASIS Is a complex of homeostatic reactions, which result in arrest of bleeding from damaged...

1
HEMOSTASIS• Is a complex of homeostatic reactions, which result in arrest of bleeding
from damaged blood vessels (hemo = blood, stasis = standing)
• Is counter-balanced by reactions, which prevent blood coagulation in uninjured vessels and maintain the blood in a fluid state– Balance between procoagulants and anticoagulants
• 4 overlapping processes or stages– Local vasoconstriction– Formation of a platelet plug– Formation of a web of fibrin proteins that penetrate and surround the
platelet plug – blood coagulation or clotting – Clot retraction.

2
LOCAL VASOCONSTRICTION• Results from
– Release of vasoconstrictor substances (paracrine & autocrine agents) from
• Platelets (i.e., serotonin & thromboxane A2) • Traumatized tissue
– Local myogenic spasm initiated by direct tissue damage– Reflex vasoconstriction initiated by activation of nociceptors and
other sensory endings
• Effects– ↓ blood flow and Pressure in the damaged area
Last for many minutes or even hours, during this time the ensuing processes of platelet plugging and blood
coagulation can take place

3
FORMATION OF A PLATELET PLUG (temporary
hemostatic plug, white plug) Damaged blood vessel wall
Collagen fibers are exposed to the blood and coated with vWF*
Adhesion of the platelets
Platelet release reaction & activation
Platelet aggregation & plug retraction
Local vasoconstriction
Intact blood vessel wall
Temporary hemostatic (platelet) plug
Secretion of prostacyclin & nitric oxide
+ stimulation- inhibition
+
+
-
-
-
Factors that prevent/limit formation of a plug
1. Prostacyclin (prostaglandin I2).Inhibits platelet aggregation; vasodilator
2. Nitric oxide* (NO).Inhibits platelet adhesion, activation and aggregation and stimulates local vasodilation
* Von Willebrand factor, a protein synthesized by endothelialcells and megakaryocytes, enhances platelet adherence by forming a bridge between cell surface receptors and collagen in the subendothelial matrix.

4
FORMATION OF A PLATELET PLUG (cont.)Stage 1. Platelets adhesion
vWF binds to glucoprotein Ib receptors of platelets and to collagen
Failure of this step may be due to:- Absence of von Willebrand factor - Malfunction of collagen - Scurvy
A. vWF - von Willebrand factor (soluble plasma protein) binds to collagen of subendothelial matrix
B. vWF exposes multiple intrinsic binding sites for the platelet specific membrane glycoprotein Ib (GPIb)

5
FORMATION OF A PLATELET PLUG (cont.)Stage 2-3 Platelets release reaction and activation. Binding of the platelets to the collagen → Release of agents from secretory granules (degranulation) – serotonin, adrenaline, several clotting factors, thromboxane A2, tissue factor and ADP Serotonin, adrenaline and ADP act locally → changes in the metabolism, shape, and surface proteins of the platelets.
Serotonin and thromboxane A2 stimulate local vasoconstriction

6
FORMATION OF A PLATELET PLUG (cont.)
• ADP and thromboxane A2 stimulate adhesion of the next layers of platelets (recruitment) through a positive feedback mechanism and formation of a platelet plug inside the vessel
Failure of this step:- Insufficient number of platelets - Dysfunctional platelets (prior activation
occurs during cardiopulmonary bypass, storage, exposure to aspirin, uraemia and acute and chronic alcohol exposure)
Stage 4: Recruitment and loose platelets aggregation

7
FORMATION OF A PLATELET PLUG (cont.)
Stage 5- irreversible platelet aggregation
• Destruction of the platelets membrane (stimulated by thrombin) → release of BAS from thrombocytes → secondary vasoconstriction
• Release of factor 3 (platelet thromboplastin) facilitates activation of blood coagulation
Stage 6. Plug retraction
• Contraction of actin and myosin in the aggregated platelets → compression and strengthening of the platelet plug


9
BLOOD COAGULATION (CLOTTING)• Is the transformation of the blood into a solid gel (a clot or thrombus)
• Occurs locally around the platelet plug; supports and reinforces the plug
• Requires 12 plasma clotting factors and 12 platelet clotting factors
• Involves a cascade of biochemical reactions in which each factor that is activated in turn activates the next factor
• The fundamental reaction is conversion a soluble protein, fibrinogen to an insoluble protein, fibrin

10
PLASMA CLOTTING FACTORS
In coagulation a series of plasma proteins called blood-clotting factors play major roles.
Most of these are inactive forms of proteolytic enzymes.
When converted to the active forms, their enzymatic actions
cause the successive, cascading reactions of the clotting process.

11
3 PHASES OF BLOOD COAGULATION• Formation of a complex of activated substances - prothrombinase
(prothrombin activator)
• Formation of active thrombin from prothrombin– Is catalyzed by prothrombin activator
• Formation of insoluble fibrin from soluble fibrinogen– Is catalyzed by thrombin

12
PHASE 1 – FORMATION OF PROTHROMBINASE
Intrinsic pathway: Starts with trauma to the blood cells or blood contact with collagen of a traumatized vascular wall.Blood contains all factors, which are necessary for coagulation. Is slow (1-6 min).
Is divided into 2 pathways
Extrinsic pathway: Starts with contact of blood with a traumatized vascular wall or extravascular tissues.Requires a cellular element outside the blood – tissue factor (tissue thromboplastin).Is fast and explosive (15 sec).
Prothrombinase

13
PHASE 2 – FORMATION OF ACTIVE THROMBIN
Prothrombinase
Thrombin- Catalyses the formation of fibrin- Activates factor XIII- Promotes platelets activation and aggregation- Activates protein C, which inactivates factors VIIIa and Va- Synthesis in the liver requires vitamin K
Contributes to the activation of factors XI, VIII (intrinsic pathway) and V – positive feedback effect on its own formation

14
PHASE 3 – FORMATION OF FIBRIN• Thrombin catalyses release of 2
pairs of polypeptides from each fibrinogen molecule and formation of fibrin monomers– Ca++ and platelet factors are
also required
• Monomers join together to form insoluble fibrin polymers – a loose mesh of stands
• Stabilization of fibrin – formation of covalent cross-bridges, which is catalyzed by factor XIII (+ Ca++)

15
FINAL EVENTS OF HEMOSTASIS• Fibrin forms a meshwork, which supports
the platelet plug
• Clot occludes the damaged blood vessel and ↓ or stops bleeding
• Retraction of the clot due to contraction of fibrin fibers and contractile proteins of the platelets – ↑ clot density– Occlusion of the damaged vessel– Bringing the edges of wound together
→ facilitation of wound heeling
• Fate of the blood clot– Invasion by fibroblasts → formation of
connective tissue through the clot– Fibrinolysis and destruction of the clot

Figure 16-10
Overview of Hemostasis and Tissue RepairDamage to
wall ofblood vessel
Tissue factorexposed
Intact bloodvessel wall
Reinforcedplatelet plug (clot)
Fibrin slowlydissolved by
plasmin
Clot dissolves
Collagenexposed
Platelets aggregateinto loose platelet
plug
Temporaryhemostasis
Cell growth andtissue repair
Vasoconstriction
Platelets adhere and
releaseplatelet factors
Thrombinformation
Coagulationcascade
Converts fibrinogen
to fibrin

17
ROLE OF VITAMIN K IN CLOTTING • Vitamin K acts as a cofactor of the enzyme γ-glutamyl carboxylase
• Is required for γ carboxylation in the liver of – Prothrombin and factors VII, IX and X – Proteins S and C (natural anticoagilants)
• γ carboxylation (introduction of a carboxylic acid group) of certain glutamate residues in target clotting factors → binding sites for Ca++ and PF3
• most of clotting factors are synthesized by the liver. Therefore, liver diseases (i.e., hepatitis, cirrhoses, atrophy) depress the clotting system. Decreased dietary intake of vit K has limited consequences on blood clotting because Vit K is continuously synthesized by the intestinal flora. Note that Vit K is fat soluble and requires fats for absorption. Lack of the bile decreases fat digestion and absorption.

18
ROLE OF Ca++ IN COAGULATION
• Ca++ is required for all steps of coagulation (except first 2 steps of the intrinsic pathway)
• ↓ in the plasma [Ca++] below the threshold level for clotting → ↓ blood clotting by both pathways

19
ROLE OF THE PLATELETS IN COAGULATION
Activated platelets
• Display specific plasma membrane receptors that bind several of the clotting factors → several cascade reactions take place on the surface of activated platelets
• Display phospholipids (platelet factors), which act as cofactors of the bound clotting factors

20
ROLE OF THE LIVER IN BLOOD COAGULATION
• Synthesis of the plasma clotting factors
• Synthesis of the bile salts, which are required for intestinal absorption of lipid soluble vitamin K

contact activation pathway
tissue factor pathway
formerly known as the intrinsic pathway
formerly known as the extrinsic pathway

22
FIBRINOLYTIC SYSTEM
• Fibrin is digested by an enzyme, plasmin (fibrinolysin) into fibrin degradation products
• Plasmin also degrades factors Va, VIIIa and GPIb
• In the blood, plasmin is present as an inactive precursor, plasminogen
• Plasminogen is activated by plasminogen activators– Adrenaline, urokinase,
thrombomodulin-thrombin complex, kallikrein, tissue plasminogen activators (t-PAs)
• t-PAs are secreted by the endothelial cells
• urokinase is produced by kidney.
Plasminogen activators
Plasminogen Plasmin
Fibrin Soluble fibrin fragments
Fibrinolysis - dissolution or disposal of blood clots

23
Fibrinolysis Clinical application-
Human t-PA is produced by recombinant DNA technology and available for clinical use. lyses clots in the coronary arteries if given to
patients soon after the onset of myocardial infarction.
Streptokinase(from bacteria-streptococcci) and urokinase are also fibrinolytic enzymes used in the treatment of early myocardial infarction

24
ANTICLOTTING MECHANISMS
• Removal of activated clotting factors from the blood by the liver
• Factors that reduce the adhesiveness of platelets– The smooth lining of the intact vessel walls– Mucopolysaccharides on the surface of endothelial cells
(glycocalyx) – repulsion of clotting factors and platelets– Circulation of the blood– Antiplatelet-aggregation effect of the prostacyclin by the intact
endothelial cells

ANTICLOTTING MECHANISMS: Natural anticoagulants
• Antithrombin III (antithrombin-heparin cofactors)– Is a plasma α globulin – its binding to heparin increases its activity.– Inactivates thrombin and some other clotting factors (IX, X, XI,
XII)
• Heparin– Is produced by the mast cells and blood basophils
By itself, it has little or no anticoagulant property, but when it combines with antithrombin III, it increases a hundred-fold the
effectiveness of antithrombin III
• Activated protein C – Inactivates factors Va and VIIIa and activates plasminogen

26
NATURAL ANTICOAGULANTS (cont.)
Endothelial cell
Thrombomodulin
Thrombin
Protein C
Activated Prot C
Protein S
VIIIa VIIIInactivation of inhibitors of plasminogen activator
Va V
Plasminogen Plasmin
Thrombin Fibrinolysis
Thrombin/thrombo-modulin/protein C pathway
Thrombomodulin is a thrombin-binding endothelial cell receptor
Binds thrombin and inactivates it
Complex of thrombin+thrombo-modulin binds protein C and activates it
Protein C in collaboration with protein S inactivates factors Va and VIIIa and activates plasminogen and fibrinolysis

27
ANTICLOTTING MECHANISMS: SUMMARY
Tissue factor pathway inhibitor
AT III-Heparin
Proteins C & S

28
DRUGS THAT INHIBIT BLOOD CLOTTING (ANTICOAGULANTS)
• Heparin
• Coumarin derivatives (i.e., warfarin) – Block stimulatory effects of vitamin K on synthesis of clotting
factors II, VII, IX, and X by the liver (inhibit epoxide reductase which activates vit K in the liver: K → K1)
• Aspirin – Low doses inhibit prostaglandins and thromboxanes synthesis
by the platelets → inhibition of platelet release reaction and platelet aggregation
– Is effective in preventing of heart attack and reduction of the incidence of sudden death

29
IN VITRO INHIBITION OF BLOOD CLOTTING• Keeping of blood in seliconized containers – prevention of contact activation of
platelets and factor XII
• Substances that bind ionized calcium to produce un-ionized calcium compound or to form insoluble salts with calcium – Sodium citrate or oxalate– Ammonium or potassium citrate– EDTA (ethylenediaminetetraacetic acid)
• Is ability to "sequester" di- and tricationic ions (Ca2+ & Fe3+)• Is widely used as an anticoagulant for blood samples for complete blood
count/full blood examination
• Heparin

30
PROTHROMBIN TIME (protime, PT test)• Measures the clotting time of
plasma from the activation of factor VII, through the formation of fibrin clot
• Assesses the integrity of the extrinsic/tissue factor pathway and common pathways of coagulation (factors VII, X, V, II, I)
• The PT test is widely used to monitor patients taking anticoagulants as well as to help diagnose clotting disorders

31
PROTHROMBIN TIME (cont.)• Depends on [prothrombin] in the blood
• Normal range 12 – 14 sec
• Increased– ↓ prothrombin (less than 10% of normal)– Deficiency of fibrinogen or factors V, VII, or X – Therapeutic anticoagulants (i.e., heparin,
warfarin, aspirin), some drugs (i.e., antibiotics, anabolic steroids, estrogens, etc.)
– Liver diseases– Vit K deficiency – Disseminated intravascular coagulation
• Decreased– Vit K supplementation– Thrombophlebitis

32
ACTIVATED PARTIAL THROMBOPLASTIN TIME
(aPTT) • Assesses the integrity of the intrinsic and common pathways
of coagulation
• Measures the clotting time of plasma, from the activation of factor XII by a reagent through the formation of fibrin clot
• Normal range 25 – 38 sec
• Prolonged time– Use of heparin– Antiphospholipids antibodies– Coagulation factors deficiency (intrinsic and common pathways; i.e.,
hemophilias)

33
2 TYPES OF ABNORMALITIES OF HEMOSTASIS
• Excessive bleeding (hemorrhagic disease) caused by deficiency of a clotting factor/s or platelets
• Excessive clotting: thrombosis, embolism, disseminated intravascular coagulation

34
CONDITIONS THAT CAUSE EXCESSIVE BLEEDING
• Vitamin K deficiency
• Deficiency of clotting factors (i.e., hemophilia)
• Deficiency of thrombocytes – thrombocytopenia
• Deficiency of von Willebrand factor

35
VITAMIN K DEFICIENCY• Results from
– ↓ intestinal absorption of fats due to ↓ bile secretion (i.e., liver disease or obstruction of the bile ducts)
– ↓ dietary intake of vit K (limited importance)
• Results in – ↓ hepatic gamma carboxylation of
• Prothrombin• Factors VII, IX and X• Protein C and S
– Bleeding tendency• Prolonged prothrombin time and partial thromboplastin time• Normal platelets count and serum fibrinogen split products

36
HEMOPHILIA• Is a hemorrhagic disease that results from deficiency of – Factor VIII (the
smaller component) - hemophilia A or classical
– Factor IX – hemophilia B, Christmas disease
– Factor XI – hemophilia C
• Is a genetic disease– Hemophilia A and B
are sex linked (X chromosome)
• Occur in males• Females are
hemophilia carriers
• Results in ↑ aPTT (PT, thrombocytes count, fibrin split products are normal)

37
THROMBOCYTOPENIA• Low thrombocytes count (below 50 000/m l) → poor plug formation,
deficient clot retraction, deficient platelet phospholipids, poor constriction of ruptured vessels → bleeding tendency from many small venules and capillaries
• Multiple hemorrhages in the skin and mucous membranes – thrombocytopenic purpura– Petechiae – small punctate hemorrhages(1-3 mm)– Echymoses - large hemorrhages (bruises)
• Other causes of purpura– ↓ plasma level of 1 or more clotting factors– ↑ fragility of capillary walls (congenital, Vit C deficiency,
adrenal failure, toxins, drugs, allergic reactions)

38
von Willebrand’s disease
• Is the most common genetic bleeding disorder
• Results from defect in vWF ( quantitative or functional)
• Results in combination of– Platelet function abnormality (vWF) - impaired adhesion– Clotting factor deficiency (factor VIII) - ↑ aPTT (PT is normal)

39
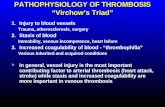
THROMBO-EMBOLIC CONDITIONS• Thrombosis - blood clotting within the CVS which obstruct the blood flow through
the CVS (Should be distinguished from extravascular clotting, clotting in wounds and clotting that occurs in the CVS after death). Thrombosis is rather a pathological condition.
• Common causes– Roughened endothelial surface (i.e., atherosclerosis, infections, traumas)– Slow blood flow– Hypercoagulobility– Acquired refers to transient or acquired conditions that increase the tendency
to clot. This might include antiphospholipid antibodies or a temporary hypercoagulable state such as pregnancy. Also, advanced carcinomas of the pancreas or lung may produce a hypercoagulable state.
– Congenital refers to hereditary conditions that increase the tendency to clot. These include Factor V Leiden, prothrombin ,protein C, protein S and antithrombin deficiencies

ConsequencesFormation of emboli (thromboembolism) – braking down of the thrombus and spreading of its particles particles throughout the CVS
Thrombosis in the left side of the heart and large arteries → emboli in the brain, kidneys, etcThrombosis in the venous system and in the right side of the heart → emboli in the pulmonary circulation

41
DESSIMINATED INTRAVASCULAR COAGULATION
• Reasons– Large areas of necrotic tissue (release of tissue factors into the blood)– Septicemia (activation of clotting by circulation bacteria and bacterial
toxins)
• Consequences– Consumption coagulopathy
• ↓ fibrinogen, thrombocytopenia• ↑ fibrin split products• ↑ PT and PTT

42
CHALENGE YOURSELFA baby is born prematurely at 28 weeks gestational age with a birth weight of 1200 g.
A few weeks after birth his mother noticed a bleeding tendency in the infant. Blood test revealed a low prothrombin level. Which vitamin can be given to the baby to reduce or to prevent the bleeding tendency?a. Vitamin B12b. Vitamin B6c. Vitamin Kd. Folic acid e. Vitamin A
C
Taking aspirin every day can reduce the risk of heart disease becausea. it is a powerful vasodilator b it stimulates fibrinolysis c. it prevents atherosclerosis d. it loosens atherosclerotic plaque on arterial walls e. it prevents platelet aggregation
E