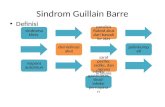
09 Cotm Guillain Barre Syndrome
-
Upload
umesh-babu -
Category
Documents
-
view
223 -
download
0
Transcript of 09 Cotm Guillain Barre Syndrome
-
7/24/2019 09 Cotm Guillain Barre Syndrome
1/4
Journal of The Association of Physicians of IndiaVol. 63November 201560
a patient presenting with a GBS-like
illness due to a SLE vasculitic flare who
was subsequently found to be also a
case of acute intermittent porphyria.
Case Report and Discussion
A 35-yr old female, came to the
emergency medica l services with
complaints of weakness of all four
limbs, difficulty in swallowing and
hoarseness of voice since 15 days.
The weakness was acute in onset
involving the lower limbs followed by
upper limbs with difficulty in getting
up from squatting and lying down
position. The weakness progressed
rapidly over one week with complete
quadriparesis. There was difficulty in
buttoning of clothes and in rais ing arms
above her head. She also developed
tingling and numbness in the hands
and feet. Weakness progressed further
and her voice became hoarse and she
was unable to swallow. There was no
history of fever, loose motions, cough
or any recent vaccination prior to the
onset of weakness. There was no history
of backache, shooting pain, altered
Guillain Barr Syndrome, Systemic Lupus Erythematosus andAcute Intermittent Porphyria A Deadly Trio
Ankita D Patil1, Niteen D Karnik2, Milind Y Nadkar3, Vishal A Gupta4, Krithika Muralidhara5,
Suresh Passidhi1
sensorium, or any flexor spasms.
There were no similar complaints in
the past. Patient had a history of joint
pain with swelling, involving both
the wrist joints and elbow joints four
years ago for which she was evaluated
at a private hospital and diagnosed
to have granulomatous synovit is .
She was then put on antitubercularmedication for six months comprising
Isoniazid, Rifampicin, Pyrazinamide
and Ethambutol for 2 months (Intensive
phase) followed by Isoniazid and
Rifampicin for 4 months (Continuation
phase). The symptoms recurred a year
later and she underwent a synovectomy
with histopathology suggestive of
tuberculous synovitis and the synovial
t issue grew MDR-TB (Mult idrug
resistant M. tub ercu lo sis) in MGIT
(Mycobacterium growth indicator
tube). She was started on treatment
for MDR-TB comprising of InjectionKanamycin 500mg OD, Tab Ethionamide
250mg BD, Tab Pyrazinamide 1500
mg OD, Tab Ethambutol 800 mg OD
and Tab Cycloserine 250 mg BD. She
took this treatment for two years and
had completed it two months prior
to presentation. Patient was also a
known case of hypertension since five
years on Tab Amlodipine and also of
bronc hial asthm a on irregular rescue
therapy with inhaled bronchodilators.
She had recurrent oral ulcers and
dryness of mouth since three months
and her ANA (anti-nuclear antibody)
test done at a private hospital was
found to be positive with a titre of
1:120 (homogenous pattern). Her family
history was noncontributory.
At presentation, she had a pulse
rate of 108 beats/min, blood pressure
of 180/110 mm of Hg, respiratory rate
of 20 per min with a single breath
1Resident; 2Professor and In-charge MICU; 3Professor and In-charge Rheumatology Services, 4Assistant Professor, 5Critical Care
Fellow, Department of Medicine, Seth GS Medical College and KEM Hospital, Mumbai, Maharashtra
Received: 07.10.2015; Accepted: 12.10.2015
C A S E O F T H E M O N T H
Introduction
In 1 9 5 2 , W o l f r a m e t a l f i r s td e s c r i b e d a c a s e o f S y s t e m i cLupus Erythematosus (SLE) who
later on developed acute intermittentporphyria. 1A study from Mayo Clinic
comprising of 676 cases of porphyria,
which were followed up for a period of
20 years, showed that SLE was present
in 2.2%. 2 Coexistence of SLE with
porphyria has been documented by
Harris et al in Arch Internal Med way
back in 1966.3Haendchen et al reported
a case of lupus who developed bullous
lesions compatible with porphyria
cutanea tarda during treatment with
chloroquine.4 Filiotou et al reported
a case of acute intermittent porphyria
(AIP) with SLE in 2002.5Sensorimotorquadriparesis in a suspected case
of SLE could be due to a Guillain
Barr syndrome (GBS)-like illness,
mononeuritis multiplex presenting
as plexopathies, an anterior spinal
artery syndrome presenting as acute
transverse myelitis or hypokalemic
periodic paralysis related to a coexistent
Sjogrens syndrome with renal tubular
acidosis. Reviewing the literature,
GBS as an initial presentation of SLE
has been reported in a few cases with
prevalence of 0.6-1.7%.6 We describe
Abstract
Peripheral nervous system involvement occurs in 3-18% patients of systemic lupus
erythematosus (SLE) cases. American College of Rheumatology (ACR) includes
19 neuropsychiatric syndromes for diagnosis of SLE divided into neurological
syndromes of central, peripheral and autonomic nervous systems along with
the psychiatric syndromes. Sensorimotor quadriparesis in a suspected case of
SLE could be due to a Guillain Barr (GBS)-like illness, mononeuritis multiplexpresenting as plexopathies, an anterior spinal artery syndrome or it can present
like an acute transverse myelitis or hypokalemic periodic paralysis related
to Sjogrens syndrome with renal tubular acidosis. We here report a case of a
fulminant quadriparesis due to a SLE flare which subsequently was also found
to be a case of Acute I ntermittent Porphyria.
-
7/24/2019 09 Cotm Guillain Barre Syndrome
2/4
Journal of The Association of Physicians of IndiaVol. 63November 2015 61
Fig. 1: Foleys catheter showing pinkurine
count of 16 per minute. She was pale.
There was no rash, joint tenderness or
swelling, cyanosis, lymphadenopathy
or icterus. On central nervous system
examination she was alert, conscious
and oriented. She had bilateral lower
motor neuron type of facial weakness,
palatal weakness with poor gag reflex.
Neck flexor weakness was present.
Motor system examination revealed
distal wasting of bilateral lower limbs
with decreased tone in both the upper
and lower limbs. The power was grade
3/5 in the proximal and gr ade 2/5 in the
distal upper limb muscles and grade
zero in the lower limbs. Superficial
and deep tendon reflexes were absent.
Sensory system examination revealed
loss of touch, pain and temperaturesensations by 50% in glove and stocking
distribution over both upper and lower
limbs. The vibration and joint position
sense were preserved. Rest of the
systemic examination was normal.
She was admitted in the medical
i n t e n s i v e c a r e u n i t . A c l i n i c a l
diagnosis of Guillain Barr syndrome
(GBS) with bulbar involvement and
impending respiratory involvement
was made. The background history of
hypertension, bronchial asthma and
evidence of distal muscle wasting in
lower limbs (motor polyneuropathy)
necessitated considering differentials
o f m ic r o s c o p ic p o lya n gi i t i s a n d
eosinophilic granulomatosis withpolyangiitis (EGPA). She had incidental
ANA t i t re o f 1 :120 (homogenous
pattern) with oral ulcers and dry
mouth; a possibility of background
systemic lupus erythematosus (SLE)
with vasculitic flare producing GBS-like
illness was considered. Her two years
history of MDR tuberculosis treatment
which ended two months prior to
the current illness also brings in the
picture, a possibility of drug-induced
lupus.
Her investigations at presentationare shown in Table 1.
She had anemia with elevated
erythrocyte sedimentation rate (ESR)
and C Reactive protein (CRP) levels.
Tests for HBsAg, Anti-HCV and HIV-1
and 2 by ELISA were negative. Urine
for porphyrins (done as a part of a
routine workup for every case of GBS)
was negative. Her electromyogram and
nerve conduction study (EMG-NCS)
was suggestive of severe sensorimotor
a x o n a l p o l y r a d i c u l o n e u r o p a t h y
affecting both upper and lower limbs
suggestive of acute motor sensory axonalneuropathy (AMSAN) variant of GBS .
CSF study revealed proteins of 14 mg%,
sugars 60 mg% with 2 lymphocytes/
mm 3. The pat ient was s tarted on
intravenous immunoglobulins (IVIg)
with a dose of 0.4 gm/kg/day for 5
days. Her autoimmune workup was
sent. On the second day of admission,
she developed tachypnea and her
single breath count dropped to eight.
She was intubated and put on invasive
vent i la t ion with FiO2 ( fract ion of
inspired oxygen) requirement of 50%
and PEEP (positive end-expiratory
pressure) of 5 cm. The autoimmune
workup reports obtained a day later is
given in Table 2.
The ANA was now positive with
very high titres (1:2560), homogenous
p a t t er n w i t h a n t i - d s D N A b e in g
positive with titres of 1:160. C3 and
C4 levels were low. The 24-hrs urine
protein was 1 gm and her d irect
Coombs test was positive. A clinical
diagnosis of SLE flare with vasculitis
presenting as GBS-like illness was
made. Anti-histone antibodies were
negative ruling out drug-induced
lupus. The pANCA positivity with
titres of 1:160 in the present scenario
was considered as secondary to SLE.
Possibility of microscopic polyangiitis
was considered; however, with high
titres of ANA and dsDNA, low C3 and
C4, microscopic polyangiitis (MPA) was
less likely. Although patient had history
of asthma, there was no eosinophilia,
hence eosinophilic granulomatosis withpolyangiitis (EGPA) was unlikely.
Patient was started on Injection
Methylprednisolone (MPS) 1 gm for 5
days along with hydroxychloroquine
2 0 0 m g O D f o l l o w e d b y o r a l
prednisolone 1 mg/kg/day. Patients
power improved over the next seven
days to grade 4 in the upper limbs
and grade 2 in the lower limbs and
the process of weaning from ventilator
was initiated. Her urine was noticed
to be persistently pink (Figure 1). A
repeat urine test for porphobilinogen
sent on day five at our hospital was
negative. However on day eleven of her
admission, we repeated the complete
panel for screening and confirmatory
tests for porphyria. The results are
given in Table 3.
UV fluorescence was used as a
screening test but it detects only
uroporphyrins and coproporphyrins
but not porphobilinogen (PBG). This
test was negative in our case on two
occasions. Hoeschs test (screening test)
is performed with Ehrlichs reagent
which gives a cherry-red colour whenmixed with PBG containing urine.
Watson Schwartz test (confirmatory
test) is performed only if Hoeschs test
samples are positive and uses saturated
sodium acetate solution along with
chloroform and butanol in addition to
Ehrlichs reagent used in Hoeschs test.7
This brought into the differential
d ia gn o s is a p o s s ib i l i t y o f a c ut e
intermittent porphyria presenting
w i t h G B S - l i k e i l l n e s s . S h e w a s
kept euglycemic (on ora l glucose
and intravenous dextrose). Injection
Table 1: Investigations at presentation
Hb 8.4 gm/dl
TLC 5800/mm3
Dierential count N77 L21 M02 E00
Platelets 2 lakhs/mm3
BUN 14.0 mg/dl
Serum creatinine 1.2 mg/dlSerum sodium 140 mmol/l
Serum potassium 3.6 mmol/l
Random blood sugar 96 mg/dl
Total protein 5.8 gm/dl
Serum albumin 2.4 gm/dl
SGOT 15 IU/l
SGPT 5 IU/l
ESR 90 mm/hr
CRP levels 120 mg/dl (N: 0 -10mg/dl)
Urine routineexamination
2+ protein, largenumber of RBCs
Table 2: Autoimmune workup
ANA Positive, homogenouspaern, 1:2560
Anti-dsDNA Positive with 1:160 titres
Anti-histone antibodies Negative
C3 Low 37 mg% (N 80-180)
C4 Low 5 mg% (N 10-40)
pANCA Positive with 1:160 titres
Direct Coombs test Positive
24-hrs urine protein 1 gm
Table 3: Tests for Urine Porphyria
UV uorescence (screening test) Negative
Hoeschs test (screening test) Positive
Watson Schwar (conrmatory test) Positive
-
7/24/2019 09 Cotm Guillain Barre Syndrome
3/4
Journal of The Association of Physicians of IndiaVol. 63November 201562
Hematin is not available in India;
hence was not given. Amlodipine and
Hydroxychloroquine were stopped in
view of porphyrogenic potential. Care
was taken to avoid porphyrogenic
drugs. Patient could be weaned off the
ventilator by Day 15.
She had responded to the treatment
( IVIg, In j . MPS fo l lowed by ora l
p r e d n i s o l o n e ) a n d h e n c e c o u l d
be we aned of f the ve nti lator with
improving power in both the upper
and lower limbs. She was switchedto metal tracheostomy tube by Day
30. Her antihypertensive medications
were changed to Tab. Telmisartan.
Metoprolol and clonidine were given
to control her autonomic disturbances.
Over the next month, her power in the
lower limbs persisted to be grade 2,
she had general debility and attempts
to close the metal tracheostomy tube
were unsuccessful. In view of her
general condition, kidney biopsy was
deferred. She developed a left lower
lobe consolidation on Day 45 and
grew Acinetobacter species which was
sensitive only to Colistin. We were
compelled to start Colistin (safety
profile for porphyria unknown). She
eventually required ventilator support
and developed autonomic disturbances
in the form of tachyarrhythmias and
had an episode of cardiac arrest needing
cardiopulmonary resuscitation. This
was followed by sepsis and acute
oligoanuric renal failure to which she
succumbed on Day 60 of MICU stay.
Thus, our patient presented with
fulminant quadriparesis with bulbar
and respiratory muscle involvement.
H e r n e r v e c o n d u c t i o n s t u d i e s
supported a diagnosis of AMSAN.
Seventy percent of GBS cases have
a preceeding history of an upper
respiratory infection or gastroenteritis
(et io logies - Campylobacter je juni,
human herpes virus, and Mycoplasma
pneum oni a) or recent immunizations,
which she lacked.
An ANA positivity of 1:2560 with
Anti-dsDNA positivity of 1:160 with
low levels of C3 and C4 clinched the
diagnosis of SLE with vasculitic flare
presenting as a GBS-like illness. An
ANA positivity after two and half
years of antitubercular treatment (6
months of Category I and two years
of MDR tuberculosis regimen) brings
a differential of drug-induced lupus.The differences between SLE and drug-
induced lupus are outlined in Table 4.
Drug-induced lupus is seen in older
age group and usually is associated
only with skin manifestations; central
nervous system and renal involvement
are very rare. A kidney biopsy would
have been helpful to differentiate
lupus nephritis from renal involvement
of MPA which would have been
pauciimmune in nature.
P e r i p h e r a l n e r v o u s s y s t e m
involvement occurs in 3-18% patientsof Systemic Lupus Erythematosus.8
GBS is classified under the peripheral
n er v e in v o lv em en t b ut i s r a r e ly
reported. Okoh HC et al have reported
a case of SLE presenting as a Miller
Fischer variant of GBS as the primary
manifestation of SLE in 2015 in Jamaica. 8
Laarhoven et al reported a case of GBS
as a presenting feature in a patient with
lupus nephritis.6
AIP is known to present with
a G B S - l i k e i l l n e s s a l o n g w i t h
autonomic dysfunction, abdominal
pain, convulsions, tachycardia and
h y p e r t e n s i o n . T h e n e u r o l o g i c a l
presentation comprises of symmetrical
muscle weakness with aref lex ia ,
sensory symptoms in the form of
paresthesias and tingling numbness in
the glove stocking regions along with
cranial neuropathies.9UV fluorescence
used as a screening test, was negative
on two occasions. This test detects only
uroporphyrins and coproporphyrins
but not porp hobi linogen (PBG). The
Hoeschs test and the confirmatory
Watson Schwartz test clinched the
diagnosis of porphyria in our patient.
What precipitated porphyria in this
case is debatable. She was on amlodipine
for five years and had received two and
half years of antitubercular therapy.
She was put on hydroxychloroquine
on diagnosis of SLE. All these arepotentially porphyrogenic drugs.10
The most common drugs precipitating
porphyria are listed in Table 5.
Does an association really exist
b e t ween p or p h yri a a nd SLE ? T o
investigate this association, Allard
et al investigated 38 patients with
various types of porphyrias for clinical
evidence of a connective tissue disease.11
Antinuclear antibodies (ANAs) were
found in 53% (8/15) patients with acute
intermittent porphyria. These patients
were more likely to have had a recent
acute attack of porphyria. Antinuclear
antibodies were not found in any
patients with any of the other types of
porphyria. Haendchen et al reported a
case of lupus who developed bullous
lesions compatible with porphyria
cutanea tarda during treatment with
chloroquine.4
The reasons o f the associa t ion
b e t wee n SL E a n d p or p h yr i a a r e
unknown. Harr is and co l leagues
proposed that porphyria can trigger
an immune response favouring SLE. 3
The accumulat ion of porphyrins
Table 4: SLE vs drug-induced SLE
Features SLE Drug-inducedlupus
Clinical
Age of onset 20-30 yrs 50-70 yrs
Gender F:M::9:1 F:M::1:1
Ethnic ity Blacks > whites Whites > blacks
Systemsinvolved
Frequentlyinvolveskidney or CNS
Rarely involves
Skinmanifestations
In >75% cases 25% only
Raynaudsphenomenon
In >95% cases 25% only
Course Indolent Limited*
Laboratory
Anti-histoneantibodies
High in 50%cases
>95%
Anti-dsDNAantibodies
High in 80%cases
Rarely high
C3 and C4 Decreased Normal
*Usually resolves over several weeks after
discontinuation of the oending medication
Table 5: Common unsafe drugs in porphyria
Porphyrogenic drugs
Documented Probable Possible
Clindamycin Amlodipine Hydroxychloroquine Escitalopram
Nitrofurantoin Atorvastatin Indomethacin Multivitamins
Phenytoin Ceftriaxone Prednisolone Glimepiride
Rifampicin Zidovudine Linezolid GlipizideIsoniazid Diazepam Clopidogrel
Cotrimoxazole Diclofenac Methlyprednisolone
Spironolactone Diltiazem Cyclophosphamide
Valproic acid Tetracyclines Metronidazole
Fluconazole Midazolam
Tramadol Telmisartan
Voriconazole Doxycycline
-
7/24/2019 09 Cotm Guillain Barre Syndrome
4/4
Journal of The Association of Physicians of IndiaVol. 63November 2015 63
causes activation of the complement
system and increases neutrophil
chemotaxis when there is exposure
to ultraviolet rays. Porphyrins can
also cause tissue damage leading to
release of autoantigens that serve as
a source for antibody formation. Pre-
existing lupus can result in an acquired
metabolic fault leading to porphyria,
and lupus precipitating a genetically
determined metabolic fault can result
in porphyria.12 An interesting fact is
that both SLE and porphyrias have
a predisposing genetic component
situated on the same chromosome.
The gene for the decarboxylase of
the uroporphyrinogen (UROD), the
enzyme deficient in cases of porphyria
cutanea tarda (PCT) is located on
chromosome 1 (1p34) and the region
1q41-1q42 has been associated withSLE. Hence, although uncommon the
association between porphyria and
lupus deserves attention.
In our case, it could be postulated
that one or more of the drugs that
the patient was exposed to prior to
her acute presentation could have
resulted in accumulation of porphyrins.
These could have produced tissue
damage leading to release of auto
ant igens . The genet ic associa t ion
outlined above could have resulted
in these autoantigens precipitating a
GBS-like illness as a manifestation of a
fulminant SLE flare.
Conclusion
Guillain Barr syndrome (GBS) can
be a pr ese nt at io n of bo th sy st em ic
lup us er y t h em a t o s us ( SL E ) a n d
acute intermittent porphyria (AIP).
This case highl ights a very rare
association between porphyria and
SLE and underlines the importance
o f r ec o gn is in g t h e c o n f o un d in g
presentations especially in females of
child-bearing age.
References1. Wolfram, S. Uber Porphyrinkolik; a contribution to the
symptomatology of acute systemic lupus erythematosus.
Dermatologist1952; 3:298-300.
2. Gibson GE, McEvoy MT. Coexistence of lupus
erythematosus and porphyria cutanea tarda in fifteen
patients.J Am Acad Dermatol1998; 38:440-3.
3. Harris MY, Mills GC, Levin WC. Coexistent systemic lupus
erythematosus and Porphyria. Arch Intern Med1966;
117:4258.
4. Haendchen L, Jordo JM, Haider O, Arajo F, Skare
TL. Por phy ria cut ane a tar da and sys tem ic lup us
erythematosus.An Bras Dermatol2011; 86:173-5.
5. Filiotou A, Vaiopoulos G, Capsimali V, Stavrianeas N,
Kaloterakis A. Acute intermittent porphyria and systemic
lupus erythematosus: Report of a case and review of the
literature Lupus 2002; 11:190-2.
6. van Laarhoven HWM, Rooyer FA, van Engelen BGM,
van Dalen R, Berden JHM. GuillainBarr syndrome aspresenting feature in a patient with lupus nephritis, with
complete resolution after cyclophosphamide treatment.
Nephro Dial Transplant2001; 16,840-842.
7. Sorte K , Palandurkar K , Goyal M , Singh A L , Basak A.
Diagnosis of Porphyria by measuring metabolites of
Heme biosynthesis in correlation with clinical findings.
J Clini Diagn Res2010; 3:2031-2035.
8. Okoh HC, Lubana SS, Langevin S, Sanelli-Russo S,
Abrudescu A. A case of systemic lupus erythematosus
presenting as Guillain Barr Syndrome. Hindawi
Publishing Corporation, Case Reports in Rheumatology,
Volume 2015, Article ID 528026.
9. Pischik E, Kauppinen R. Neurological manifestations of
Acute Intermittent Porphyria. Cellular Molecular Biology
2009; 72-83.
10. Kepple A, Cernek PK. Amlodipine-induced acute
intermittent porphyria exacerbation. An na ls
Pharmacother1997; 5:13.
11. Allard SA, Charles PJ, Herrick AL, McColl KE, Scott JT.
Antinuclear antibodies and the diagnosis of systemic
lupus erythematosus in patients with acute intermittent
porphyria.Ann Rheum Dis1990; 49:2468.
12. Murata J, Shimizu T, Tateishi Y, Abe R, Shimizu H.
Coexistence of a systemic lupus erythematosus and
porphyria cutanea tarda: case successfully improved
by avoidance of sunexposure. Internat J Dermatol2006;
45:435437.