Web view: Injury or trauma for maxilla or mandible, surgery in the area, extraction of the teeth,...
Transcript of Web view: Injury or trauma for maxilla or mandible, surgery in the area, extraction of the teeth,...

Hind AlabbadiOral Pathology,Sheet 4 12\10\2014
Oral Infection \ Bacterial infection
Bacterial infection caused by Actinomyces species mostly Actinomyces israelii.
Predisposing factors : Injury or trauma for maxilla or mandible, surgery in the area, extraction of the teeth, periapical infection, pericoronitis.
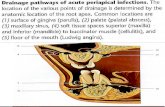
Clinical presentation: The actinomyces in the head and neck presented as Soft tissue swellings (Fig1) , you should differentiate it from other causes with such presentation. So here It's chronic swellings , very hard in the beginning but with time it become fluctuant and open with sinus or even multiple sinuses for several months then scarring will occur in that area .
So if the clinical presentation was swellings with multiple sinuses , you have to think about actinomyces.
Lymphadenopathy usually not present.
H.w :You have to think about the source of bacteria?
How to conferm your diagnosis? As we said there is opening with multiple sinuses and drainage of pus like material , so you can take this material and look on it under microscope after staining, so you can see the sulfur granules = collection of the filamentous bacteria (Fig2), or if you send it to microbiology lab for culture, it will contain growth of this type of bacteria (Fig3).That's why it is called actinomyces which mean it is resembled the fungus but it is filamentous bacteria.
Histological : Granulation tissue and in the center there where be pus formation and in the pus you can find the sulfur granules. So it is granulematus type of inflammation.
Bacterial infection caused by Trepanoma pallidum with 3 stages :
Primary syphilis: it is Genital infection but with orogenital contact the person may present with primary syphilis in the oral cavity ; lip , tongue or floor of the mouth. After the incupation period there will be firm nodule around 0.5 cm in diameter followed by ulceration, here we call it Chancre. So the Chancre is round , shallow , painless ulcer with clean base & raised indurated edges with lymphadenopathy in the region. This will stay for few weeks and there will be healing.
-it is contagious.
Page 1 of 10
Actinomycosis
Syphilis
*Note that I put some figures in the last paper of this sheet , Refer to them when needed.

Hind AlabbadiOral Pathology,Sheet 4 12\10\2014
Histological: Ulcerated granulation tissue with a dense CICI.
This will stay for few weeks followed by healing then after few weeks to month there will be :
Secondary syphilis : pt's will have non-specific signs and symptoms like mild fever, malaise, headache, sore throat with generalized lymphadenopathy and skin rash (coppery macules)
النحاس لون تشبهOrally: the pt's will have white lesions “mucous patches” which is ulceration covered by mucoid material.Some of these mucous patches will present like “Snail’s track ulcers” (Fig4) Also some of pt's will have like an eruption on buccal mucosa or angle of the mouth with surface roughness we call it “Condylomata lata”Othere pt's with papules and splitting at the angles of the mouth called “Split papule” (fig5)
-it is discharging the bacteria so it is contagious as well as the primary syphilis.
- This will stay for 2-3 weeks followed by healing then after few years there will be:
Tertiary syphilis: It can affect any organ in the body mainly cardiovascular system (vascular syphilis) and neural system (nural syphilis). Oral manifestations :1- Gumma: affect Palate, tongue or tonsils , Swelling ⇒ necrosis ⇒ painless, deep round
ulcer with perforation that may lead to oronasal communication(Fig6)Histological: granulomatus granulation with multinucleated giant cells. (Fig7)2- Atrophic glossitis: syphilis will cause obliterations of small blood vessels with atrophy to
the mucosa like the dorsum of the tongue so we call it "Atrophic glossitis"3- Syphilitic leukoplakia : That atrophy usually followed by whitish lesion or leukoplakia so
we call it syphilitic leukoplakia ,this name is not accurate because as we know leukoplakia means without known cause .There is a risk of transform it to squamous cell cancer
Congenital syphilis : Transplacental infection with various severity which can lead to : - Abortion . - Hutchinson triad: blindness, deafness & dental anomalies (Hutchinson's incisors &mulberry molar )
Page 2 of 10

Hind AlabbadiOral Pathology,Sheet 4 12\10\2014
Bacterial infection caused by Mycobacterium tuberculosis. Incedance increases after the emergence of AIDS & drugs resistance or drugs abuse.
Oral manifestations manly seen in Immuno-compromised pt . Present of bacteria in the sputum so during the cough, bacteria may deposit in the oral cavity in the tongue or vestibules causing chronic painful ulcer called "Angular ulcer" , also it may cause infection of maxilla or mandible " Chronic osteomyelitis" or pt with chronic lymphadenopathy in the cervical region
To conferme it you have to take history of TB by chest X ray or by taken biopsy, so in the hisopathology there is granulomayus inflammation and in the center there will be necrosis "caseating necrosis" with multinucliater giant cells and langerhans giant cells nuclei arrange at the periphery of the cytoplasm.
Remember: granuloma can be manifested of deferent diseases like sarcoidosis….etc , so how to confirm that is TB infection ? You have to do special stain for the bacteria in the sputum , called : Ziehl-Neelsen stain (Fig8)
Bacterial infection caused by Mycobacterium leprae. Not commen in our contry but found more in Southeast Asia, South America & India, of 2 types :
Tuberculoid leprosy Lepromatous leprosylimited or localized generalized or disseminated (more dangerus)active cell mediated immunity ↑ defect in cell mediated immunity ↓defect in antibody mediated immunity ↓
Leprosy causing a lot of disfigurement to the pt in the skin , in the oral cavity you found:
- 50% of with type 2
- Nodules → ulcers → fibrosis
- Palate, gingival and tongue
- with Facial deformity
Page 3 of 10
Tuberculosis
Leprosy

Hind AlabbadiOral Pathology,Sheet 4 12\10\2014
Oral Infection \ Fungal infection
- Fungal infection caused by Candida is more common infection in oral cavity.
Species: Parapsilosis, Tropicalis, Pseudotropicals,
Glabrata, Krusei, Guilliermondi, Albicans
Most commone one is ….. Albicans ……
-Can present in deferent form : yeast (rounded cells) Fig9A or hyphae (long branching septated, filaments like) Fig9B , The pathogenic form is the 2nd one ; i.e hyphae.
- Commensal organisms الفم داخل 40متعايشة % of healthy adult. But the chance to find Candida in the oral cavity increases more the 40% with the predisposing factors e.g. elderly pt. , pt. with systemic disease, pt. with denture .
So Predisposing factors:
Local factors Systemic disease
trauma as a result of appliances for example, denture, smoking, frequent carbohydrates intake, xerostomia ,extreme of ages as in elderly or newborn ( Immunity ↓) ,Drugs :immunosuppressant , corticosteroids and broad spectrum antibiotic.
anaemia (iron, B12 deficiency), DM (it's important, you may help in diagnosis of diabetes during history and examination), HIV, blood dyscrasia (leukemia, lemphoma, leucopenia ….) , Endocrine( hypoparathyroidism ,hypothyroidism….), Immuno ↓
- In the oral cavity, there is Specific & nonspecific immunity against Candida.
H.w\ Candida of high or low pathogenicity? Is it superficial or deep infection? Why broad spectrum antibiotic is predisposing factor for Candida infection? What is the specific & nonspecific immunity against Candida ? How Candida cause infection with damaging to the oral cavity (pathogeneses) and can it cause squamuse cell carcenoma?
Page 4 of 10
Candida
Candida did not cause ulcer.Note

Hind AlabbadiOral Pathology,Sheet 4 12\10\2014
Classification:
Group 1 : Primary-Confined to the oral mucosa ∗ Acute: Pseudomembranous (thrush) & Erythematous (atrophic)
∗ Chronic: Pseudomembranous & Erythematous; Hyperplastic (candidal leukoplakia).
∗ Candida-associated lesions: Denture stomatitis; Angular cheilitis & Median rhomboid glossitis.
Group 2 : Secondary-Oral manifestation of generalized candidiasis
∗ Systemic mucocutaneous candidosis.
Pseudomembranous (thrush):
• Acute & Chronic (in immune compromise pt's) • Clinically: -easly to diagnose الرضيع فم في المتخثر الحليب (Fig 10) يشبه-Soft, friable, creamy-colored plaques. - Wiped off → erythematous base (red or bleeding base). -Isolated small flecks or widespread plaques. -Any mucosal surface of mouth. -Asymptomatic but could be burning sensation or unpleasant taste (salty or bitter). -Infants (6-10th day after birth )& elderly. -In AIDS pt's, it is more resistant to the drugs and it can reoccurs after healing
H.w\ what is the source of Candida in infant?
• How to confirmer your diagnosis other than by Wiped off ? By smear and PASS stain and you see the bacterial form (hyphe , yeast) with desquamated epithelial cells.
• Histological: by biopsy , you will see :Hyperplasia, Parakeratosis + Candidal hyphae invading the superficial part of the epithelium at a right angle (Fig11) & inflammatory reaction (neutrophils) in the superficial part of the epithelium which may lead to mictoabsess , So this layer is weak and easily wiped off (pseudomembrane) التسمية جاءت هنا ومن
Acute & CICI in lamina propria.
Page 5 of 10

Hind AlabbadiOral Pathology,Sheet 4 12\10\2014
Erythematous candidosis:
• Acute and Chronic (in immune compromise pt's) . • Mostly at the dorsum of the tongue. • Most predisposing factors: brood spectrum antibiotics or mutable narrow spectrum drugs, systemic steroids or inhaler type in asthmatic pt. with redness at the dorsum of the tongue.
• Clinically: red oral mucosa, painful (Remember thrush was Asymptomatic) , may be generalized redness all over the mouth not merely at the dorsum of the tongue.
H.w\ Why Erythematous candidosis is painfull compared with Pseudomembranous type of candidal infection ? What are the predisposing factors for generalized form of Erythematous candidosis ?
• Histological:
thin epithelium (not parakeratosis), candidal hyphae are not alwase present , inflammatory cell infiltrate in the lamena propria.
AIDS pt may present with Angular cheilitis: redness, fissure and burning sensation at the angles of the mouth.
Chronic hyperplastic candidosis (candidal leukoplakia):
Most important type because of its prognosis, so the pt needs more follow up.
Clinically :
• Males of middle age, heavy smoker.
• Dense, white patches of irregular thickness (called leukoplakia), sometimes with some red atrophic areas (called speckled leukoplakia) .But again these names is not accurate because as we know leukoplakia means without known cause. • Mostly at anterior part of buccal mucosa with triangular in shape ,bilateral (easy to distinguish) also may present at the lateral border or the dorsum of the tongue. •pt may present with Angular cheilitis as well as chronic hyperplastic candidosis.
•How to confirmer your diagnosis to exclude Leukoplakia, Lichen planus , Squamous cell carcinoma, trauma by cheek biting or others? So it's very important to confirmer your diagnosis .
•Histopathology (biopsy) we will see :
Parakeratosis with Candidal hyphe and inflammatory reaction (neutrophils) in the superficial part of the epithelium which may lead to mictoabsess. Same as the thrush type.
Page 6 of 10

Hind AlabbadiOral Pathology,Sheet 4 12\10\2014
•Marked hyperplasia in the epithelium; so some elevation in the area climically.
•If the lesion clinically is white so you will see Marked hyperplasia, but if it was speckled (with some red areas) you will see some atrophy .
•Acute & CICI in prickle cell layer (more inflammation compare to the thrush type)
•This lesion is potentially malignant, so the most important thing is the present of Dysplasia that is found in up to 30% , but they thought that the dysplasia here is not true one, but it is caused by bacterial proliferation, so for confirmation that is true dysplasia you prescrip antifungal drug first then after 2 weeks you take the biopsy, if there is dysplasia it will be true dysplasia that may progress to malignancy, and the percentage will drop to 15 % .
So 15 % of the pt's with Chronic hyperplastic candidosis have true dysplasia But not all of them progress to malignancy . if predisposing factor↓ dysplasia ↓ then no cancer .
But in some literature they still thought that the bacteria is the cause of the dysplasia. Smoking candida dysplasia.
Candida-associated denture stomatitis
• It is candida associated lesion + trauma from the denture (complete or RPD) or removable orthodontic appliance, poor denture hygiene, roughness of the fitting surfaces of the denture, malocclusion in the denture, sleeping with the denture (no saliva reach palate).
• It is up to 50% of denture wearer. The reason behind this high % is that it is Asymptomatic clinically. • Clinically: asymptomatic erythema of the palate . • Newton's classification
Grad : Pinpoint areas (localized spots)
Grad : Diffuse area (in all coverd area)
Grad : With granularity (rednes with small polips called inflammatory papillary hyperplasia which is more chronic)
Histological:
• Candidal hyphae more growth in the fitting surfaces while parakeratosis or nonkeratenise in the palate area smear. • inflammation. • dilatation of blood vessels in lamina propria.
Page 7 of 10

Hind AlabbadiOral Pathology,Sheet 4 12\10\2014
Candida associated and other forms of Angular cheilitis:
• Bilateral erythema & fissuring at the corner of the mouth with burning sensation.
• 30% of patients with denture stumatitis , here the pt's are elderly with old denture with loss of vertical dimention then folding at the angle of the mouth with Candida infected saliva get out ,so continuses wetting of the angle of the mouth and adjacent skin which tend to infect that area.
• Some pt's do wetting of the angle of the mouth by their tip of the tongue leads to Angular cheilitis.
• May due to bacterial infection eg. Staphcocci , Beta hemoletic streptococci .
• May due to both Cnadida and Bacterial cause.
• In dr's who wear masks رطوبة the bacteria come from the nose and infect the angle of the ,منطقةmouth leads to Angular cheilitis.
• seen also in Nutritional deficiencies pt's eg: anamic pt's .
Chronic mucocutaneous candidosis:
• Not only seen in the oral cavity , it can affect other mucus membrane and in the skin ,hear and nails. • Persistent & refractory candidal infection look like Chronic hyperplastic candidiosis.
Persistent = chnonic ,, refractory = the lesion reoccure even after drug treatmen.
Five types: (refer to our reference book for more details)
1.Familial limited type localized type.
2. Diffuse type (Candida granuloma) affect skin , organ or even the oral cavity.
3. Candidosis endocrinopathy syndrome Hypoparathyroidism, Addison’s disease, hypothyroidism, DM.
How to defrentiat between Candidosis endocrinopathy syndrome (Chronic mucocutaneous candidosis) and candidal leukoblakia?
Here the pt is Young with family hestory , skin &nails lesions and endocrine disease .
4. Late-onset type (Thymoma syndrome) deficiency in cell mediated immunity.
5. CMC associated with primary immuno ↓ deficiency in immune system.
Page 8 of 10

Hind AlabbadiOral Pathology,Sheet 4 12\10\2014
• Rare fungal infection .
• Deep fungal infection.
• Cryptococcosis, Blastomycosis, Histoplasmosis, Aspergillosis.
• Nodular lesion then ulcer lesion.
• Granulomas and fungal infection by biopsy and special stanin.
• Other deep fungal infecyion affecting respiratory tract or internal organs.
Good Luck
Hind Alabbadi
Page 9 of 10
Deep mycosis

Hind AlabbadiOral Pathology,Sheet 4 12\10\2014
Figures
Page 10 of 10
Fig1 Fig2 Fig3
Fig4 Fig6Fig5
Fig7 Fig8 Fig9A
Fig9B Fig11Fig10