˘ ˇ ˆ ˆ - DiVA portaluu.diva-portal.org/smash/get/diva2:272520/FULLTEXT01.pdfThe unknown child...
Transcript of ˘ ˇ ˆ ˆ - DiVA portaluu.diva-portal.org/smash/get/diva2:272520/FULLTEXT01.pdfThe unknown child...

������������������� ���������� �����
���������� �������������� ������������������� ������� ����������������������������
��������� ����� �������������� ������� ������� ���� ������������ �� ���������� ��� ��
�� �!"�#$ �%��!
&%%!�'()'*(+,(&%-!��.�*�'*))�*.(/,*����0�1�0� 0��0�2�*',��(�

����������������������� ������� ������������������������������������ ���������������������������������� ���������������� ��������!���""#����$%&$'�(�������������(������()������������������ ��������*�+������������,������������������,�����*
��������
-�������.*��""#*�/������������)������������0���(���1������/�������������������������2����+�������*�3���� ������������ ���������*������� ���������������������������������������������������������������������������45#*�6����*� ������*������#!57#$7''47!6%"74*
)������������������������������(�������,������������������(������2����8�-�9��������*��+�������(�������������,����������������������������(�������������������������������������������������������������������:�(����������������������������,�����������������-�*)�����������,����$"#"�����������,����������'4'�������������������(��������������
���,�������������,7����������*�+���)�������;����<��������(�/��������������8)=�/<7/�9�� ������ � ������������� ��� ������������/����� (�/��������������� ������ <����8��/7�-9��,��������(���������������������������������*�+��������������������,���56�8!#�>9����?����*3�� ������������ �������� ,��� ������� �� %$�>� (� (������� ��� �� $"�>� (������*�/�?�
���������,��������������$$�>�(�(����������'�>�(������*�@����$�>�(��������?�����,���������������������������������(���(���������*�3��������������������������������8A/��B%"9�,�������:�(������(����������������,����������������:�(�����(���������������,��������������(��������*�3���������������,������������������������������������������-�7�����������:�(������,���������(���*�+����,�������������������������(�)��������8��)9�������(7������C�����������,��������(�����������(�����������������*�.����������(���������� ������� �������� ������������,��������������,���������D�������������������������,��������*3����� �?������� ,��� �� ������� ���� ���������� (� ������������� ������ ������ �(���
��������(����-�������C����������7���������������������������������,�*����������(�����-��,����������������,�����������(�����(��,�����������:����������������������������������������������(*�3�����(����(�����������������������������,�������������(�,�����������*�3�����������������(�����-�������������(�����,�����C������*�+������������(����������(�����������������,���,�������������������������������������������������������������������������������,�����������*
�����������(�����������������(������2�������������������������������������������������(���������(����-�
������� ������!��������������"����#������ �������#��������!�������������� ���$%&'()'��������!�������
E�.�����-�������""#
��� �$6'$76�"6��A �#!57#$7''47!6%"74��&�&��&��&����7$"#464�8����&DD��*:�*��D������F��G��&�&��&��&����7$"#4649

”Hoppas inte utan tvivel och förtvivla inte utan hopp”
Seneca

The unknown child
That child will never lie in me, and you Will never be its father. Mirrors must Replace the real image, make it true
So that the gentle love-making we do Has powerful passions and a parent’s trust
The child will never lie in me and make
Our loving careful. We must kiss and touch Quietly, watch our reflexions break
As in a pool that is disturbed. Oh take My watchful love; there must not be too much.
A child lies within my mind. I see
the eyes, the hand. I see you also there. I see you waiting with an honest care, Within my mind, within me bodily,
And birth and death close to us constantly.
Elizabeth Jennings (1926-2001)

List of papers
This thesis is based on the following papers, which are referred to in the text by their Roman numerals. I Volgsten H, Skoog Svanberg A, Ekselius L, Lundkvist Ö, Sundström
Poromaa I. (2008) Prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment Human Reproduction 2008; 23: 2056-2063
II Volgsten H, Skoog Svanberg A, Ekselius L, Lundkvist Ö, Sundström
Poromaa I. (2008) Risk factors for psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment Fertility & Sterility Dec 2008, in press
III Volgsten H, Ekselius L, Sundström Poromaa I, Skoog Svanberg A.
Personality traits associated with depressive and anxiety disorders in in-fertile women and men undergoing in vitro fertilization treatment. Acta Obstetricia et Gynecologica Scandinavica, Accepted for publication
IV Volgsten H, Skoog Svanberg A, Olsson P. Unresolved grief in women
and men in Sweden three years after undergoing unsuccessful in vitro fertilization treatment Submitted
Reprints were made with permission from the respective publishers.


Contents
Introduction...................................................................................................11 Infertility ..................................................................................................11 Causes of infertility ..................................................................................11 Treatment of infertility .............................................................................12 Hormone therapy during IVF...................................................................12 Stress symptoms.......................................................................................13 Crisis reactions .........................................................................................13 Grief reactions ..........................................................................................14 Psychiatric disorders in the general population........................................15 Major depression ......................................................................................16 Psychiatric disorders in infertile females and males ................................17 Risk factors for mood and anxiety disorders............................................18 Personality traits .......................................................................................19 Experiences of childlessness after the end of IVF....................................19
Aims..............................................................................................................20
Materials and methods ..................................................................................21 Study sample papers I - III .......................................................................21 Study setting papers I-IV..........................................................................21 Study design papers I-III ..........................................................................21 Psychiatric assessment .............................................................................22 Personality assessment .............................................................................23 Statistical/Data analyses papers I-III ........................................................24 Statistical/Data analyses papers II-III.......................................................24 Study design, participants and data analyses paper IV.............................24 Ethical considerations ..............................................................................26

Results...........................................................................................................27 Prevalence of mood and anxiety disorders (paper I) ................................27 Risk factors for mood and anxiety disorders (paper II)............................31 Personality traits associated with mood and anxiety disorders (paper III) .................................................................................................34 Experiences of childlessness three years after unsuccessful IVF (paper IV) .................................................................................................35
Discussion.....................................................................................................38 Methodological considerations papers I-III .............................................38 Methodological considerations Paper IV .................................................41 Main outcome findings.............................................................................43
Conclusions...................................................................................................50
Clinical implications .....................................................................................51 A midwifery perspective ..........................................................................51
Future research..............................................................................................52
Summary in Swedish – svensk sammanfattning...........................................53
Acknowledgements.......................................................................................56
References.....................................................................................................58

Abbreviations
ART assisted reproductive technology
BMI body mass index
CBT cognitive behavioural therapy
DSM IV diagnostic and statistical manual of
mental disorders, fourth edition
ESHRE european society of human
reproduction and embryology
ET embryo transfer
GAD generalized anxiety disorder
GnRH gonadotrophin releasing hormone
hCG human chorionic gonadotrophin
ICSI intra cytoplasmic sperm injection
IVF in vitro fertilization
NOS not otherwise specified
OCD obsessive-compulsive disorder
PR pregnancy rate
SET single embryo transfer
WHO world health organization


11
Introduction
Infertility Infertility is a reproductive failure and a significant loss affecting women and men. Reproductive health, according to WHO’s definition of health as a state of complete physical, mental and social well-being, addresses reproduc-tive functions at all stages of life. One of these functions is the individual’s capability to reproduce (1). The ability to have a biological offspring is an existential concern. In most cultures womanhood is considered the ability to bear and give birth to a child and creating a family is central to most couples. Therefore, reproductive failure, such as infertility, can cause reactions of crisis (2) and depressive symptoms (3). Previously it was assumed that men-tal factors such as depression caused infertility. Today, when assisted repro-ductive technology (ART) has become fairly routine, it has become apparent that the mental strain experienced by many infertile couples may be more of a consequence of infertility than a cause (3, 4). However, another hypothesis has been suggested; that there is a reciprocal relationship between mental health and infertility in that both effects may occur concurrently (5-7).
Causes of infertility Infertility is defined as the inability to conceive after one year of regular intercourse without contraception and affects approximately 10 – 15 % of all couples of fertile age in industrialized countries (8). Infertility is considered primary when the female has never conceived and secondary when the fe-male has not achieved subsequent pregnancy. Factors causing infertility can be explained by a female (such as a tubal factor, endometriosis or anovula-tion) or a male factor (such as oligo- or azoospermia). For some couples the cause can also remain unexplained after evaluation, and a complete diagno-sis may not be established before treatment. The female’s age can be the cause of infertility, as fertility declines as the quality of the ovum are af-fected by age (9, 10). Thus, postponement of the first child is causing fertil-ity problems (11, 12). In addition, there are lifestyle factors that may cause infertility, such as female obesity, smoking and psychological stress (12-15).

12
Treatment of infertility In vitro fertilization (IVF) is routine treatment today for all types of causes of infertility. IVF was introduced in 1978 when the first child was born after IVF treatment (16). The first child after IVF treatment in Sweden was born in 1982 and 10 years later fertilization by intra cytoplasmic sperm injection (ICSI) was introduced. Almost 3 000 children are born each year in Sweden after IVF, which corresponds to nearly 3 % of all newborn infants. Every third woman conceives and one out of four women has a live birth after one IVF treatment (17). Two out of three counties in Sweden offer three subsi-dized IVF attempts to the infertile couple and in the other counties one or two attempts are offered. Of couples undergoing IVF treatment between 30 - 40 % will remain childless after treatment (18, 19). At the time of the study IVF pre-treatment included follicular stimulation with daily injections of gonadotrophin (recombinant FSH), following down regulation with, in most cases, Gonadotrophin releasing hormone (GnRH) agonist (standard/long protocol) or in combination with a GnRH antagonist (short protocol). When follicular maturation was obtained, as monitored by regular examinations with transvaginal ultrasonography, oocyte retrieval was performed 34 - 36 hours after an injection of 10 000 IU hCG. Fertilization in vitro was performed either by IVF or ICSI. Embryo transfer (ET), in most cases of a single embryo (82 %), was performed 2 - 3 days later. Good qual-ity spare embryos were cryopreserved to be transferred later in subsequent cycles. Luteal support was given with intravaginal progesterone. The preg-nancy test result (hCG in urine) was assessed at home by the woman 16 - 19 days after oocyte retrieval. The couple reported the result of the pregnancy test to the clinic. The IVF treatment with a long protocol lasted approxi-mately 6 - 7 weeks from onset until the pregnancy test was assessed. Outcome after IVF treatment can be reported as pregnancy rate (PR); either as the result of the pregnancy test (biochemical pregnancy) or the result veri-fied by ultrasound (clinical pregnancy). The outcome can be reported either by treatment per started cycle or by embryo transfer (20). Few studies report the outcome as live birth rate, although a successful outcome of treatment for the infertile couple is not achieved until the result is a live birth (15, 21).
Hormone therapy during IVF Gonadotrophin releasing hormone (GnRH) is a hypothalamic hormone used for down regulation during IVF treatment to prevent premature ovulation. Adverse effects from GnRH treatment include menopausal symptoms such as hot flashes, headache and mood changes (22). The mood changes induced

13
by GnRH treatment are usually not severe enough to fulfil the criteria for major depression, and have generally been attributed to low estradiol levels (22, 23). A short protocol (antagonist) has been shown to minimize the ad-verse mood effects in comparison to the prolonged ovarian suppression induced by standard/long treatment (24, 25). Fewer self-reported short-term symptoms of depression one week after the last IVF failure were found after short compared to standard/long treatment, as prolonged ovarian suppression may cause more depressive symptoms (25), whereas no differences in de-pressive symptoms were noted between the two treatment strategies follow-ing the first IVF (26). However, the mood effects of hormone therapy during IVF have been the focus of surprisingly little study. Women usually express high expectations and hope for a successful outcome when IVF is initiated and disappointment and symptoms of depression fol-lowing treatment failure (27-30). Thus, infertility and undergoing IVF treat-ment with hormone therapy is demanding and can cause stress symptoms and emotional reactions of crisis, grief and depressive symptoms.
Stress symptoms Infertility and undergoing IVF treatment are stressful life events and can lead to stress symptoms, psychosomatic stress reactions and adjustment disorders. Adjustment disorders are more prevalent among infertile women than con-trols after evaluation and prior to fertility treatment (31). An adjustment dis-order is a maladaptive reaction to an identifiable stressful event which is assumed to diminish when the stress ceases. IVF-related stress has been con-firmed not only by psychometric measurements but also by increasing corti-sol levels throughout the treatment course (32, 33). Adjustment disorders are characterized by emotional reactions to stressful events similar to depres-sion, but they spontaneously resolve after adjustment over time without spe-cific treatment (34). However, symptoms of an adjustment disorder do not correspond to normal grief reactions. Adjustment disorders are limited to a time period of less than six months after a stressful event (35). Stressful life events are reported more frequently in females than in males and are sug-gested to increase the risk of developing major depression (36-38).
Crisis reactions Infertility is conceptualized as a major crisis in life. A crisis occurs after a stressful life event, threaten important life goals and unresolved problems from the past arise (2, 39). A crisis evoke emotional reactions that are classi-fied into four main phases; the initial phase (shock, surprise, denial), the

14
reactive phase (frustration, anger, anxiety, guilt, grief, depression, isolation), the adaptive phase (acceptance) and a resolution phase (planning for future solutions) (2, 39). Reactions during a crisis are determined by factors such as; influences of the event itself, pre-existing personality, cultural factors and social support from significant others (40). A crisis is considered a transi-tional period with opportunity for either personal growth or increased risk for development of psychiatric disorders, depending on how the crisis is handled (41). The conceptual framework of the crisis theory (2, 41) is modified for the purpose of the infertility crisis (39). Although the crisis theory may initially be used the theory is less useful for the adaptive phase as infertility may consist of recurring stressful events (42). Women who have undergone un-successful tubal surgery for a female infertility factor mostly remain in the reactive phase when interviewed two years after surgery according to Lalos and co-workers (43). The infertility crisis differs from other life crises, that are time-limited with duration of six weeks or less for the reactive phase and an adaptive phase of up to one year (2, 39).
Grief reactions Grief is a common reaction in women after a diagnosis of infertility (39). Infertility represents many losses; the loss of fertility and reproductive abil-ity, and the loss of a child and biological offspring (44). Grief is a normal reaction to a distressing situation, such as a loss (45). The duration of normal grief reactions depends on the grieving process, which is considered impor-tant for successful adjustment to the infertility crisis (39, 44, 45). However, when the loss is of a potential, not an actual loss, the couple may not realize they are allowed to grieve (39). The grieving process may be hampered or prolonged, thus causing compli-cated or pathological grief. Symptoms that are not characteristic for normal grief reactions are excessive guilt, suicidal ideation and feelings of worth-lessness (35). Complicated grief occurs when grief reactions persist more than two months after a loss and it is a psychiatric illness that requires evaluation and treatment, and is consistent with the definition of major de-pression (35). Therefore, distinguishing between grief reactions, complicated grief and depression is important but can be difficult (38, 46-48). Most clinical symp-toms are similar, except grief reactions are often self-limited and with pre-served self-esteem (46).

15
Psychiatric disorders in the general population A psychiatric disorder is, according to the American Psychiatric Association (APA), conceptualized as “a clinically significant behavioral or psychologi-cal syndrome or pattern that occurs in an individual and that is associated with present distress or disability or with a significantly increased risk of suffering death, pain, disability, or an important loss of freedom. In addition, this syndrome or pattern must not be merely an expectable and culturally sanctioned response to a particular event, for example, the death of a loved one. Whatever its original cause, it must currently be considered a manifesta-tion of a behavioral, psychological, or biological dysfunction in the individ-ual” (49). Psychiatric disorders, in this thesis, are diagnosed according to a descriptive criteria-system, the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (49).
The lifetime prevalence according to epidemiological and national-based studies of major depression varies between 10 – 25 % in women and 5 - 12 % in men whereas the point prevalence of major depression is 5 – 9 % in women and 2 – 3 % in men. The lifetime and 12-month prevalence of anxi-ety disorders varies as follow; GAD 5 % and 3 %, panic disorder 1.5 – 3.5 % and 1 - 2 %, OCD 2.5 % and 1.5 – 2 %, social phobia 3 - 13 % and 8 % respectively, in both women and men (49). The lifetime prevalence of mood disorders is approximately 24 % in women and 15 % in men and the 12-month prevalence 14 % in women and 8.5 % in men. The lifetime prevalence of anxiety disorders is approximately 30 % of women and 19 % of men and the 12-month prevalence 23 % in women and 12 % in men. The lifetime prevalence of any psychiatric disorder is 55 % in women and 49 % in men. The 12-month prevalence for alcohol abuse/dependence is 6 % in women and 16 % in men. (50-53). Furthermore, there is a substantial co-morbidity between anxiety and depres-sion in both females and males (50, 54, 55). Mood disorders are also associ-ated with increased reporting of physical symptoms such as headache, fa-tigue, back pain and bowel complaints (56).

16
Major depression Major depression is a disorder of mood or affect; mood refers to the internal emotional state and affect to the external expression of emotional experi-ences (46, 59). Major depression is two to three times as common in women as in men (60) and the peak incidence in females occurs during the reproduc-tive years, with a mean age at onset of 30 years (61). The two core symptoms of a diagnosis of a major depressive episode are either depressed mood or the loss of interest or pleasure in nearly all activi-ties. The additional symptoms are changes in appetite or weight, sleep, and psychomotor activity, decreased energy, feelings of worthlessness or guilt, difficulty thinking, concentrating, or making decisions. Recurrent thoughts of death or suicidal ideation, plans or attempts is another DSM-IV criteria for depression (49). Five or more of the symptoms/criteria have to be fulfilled according to the DSM-IV criteria and persist for most of the day, nearly every day, for at least two consecutive weeks for the diagnosis of major depression. The epi-sode must be accompanied by clinically significant distress or impairment in social, occupational, or other important areas of functioning (49). Major depression can become recurrent (new episode of depression after full remis-sion) and may substantially impair an individual’s ability to cope with daily life. Relapses (when depression is not in full remission) occur in 75 - 80 % of cases. Most cases of depression can be treated with pharmacotherapy, such as SSRI (selective serotonin reuptake inhibitors) and/or with psychotherapy. How-ever, pharmacotherapy during pregnancy is controversial and the first choice for treatment of depression in infertile females has been considered psycho-therapy, as these women are attempting to conceive and consequently should avoid medication (47). A recent review suggests that SSRI should be used with caution during pregnancy (62). However, the current recommendations in Sweden are that antidepressants should not be avoided during pregnancy (63, 64). Psychotherapy, as cognitive behavioural therapy (CBT) has been demonstrated to be an efficient treatment for depression in the general popu-lation (65) and in infertile females undergoing IVF (66, 67). CBT has also been recommended for infertile women with anxiety disorders (47). It has been predicted that major depression will be the second most common health problem and a leading cause of disease-related disability in the popu-lation by 2020 (57). Already, major depression imposes substantial impair-ment and a reduced quality of life among women throughout the world (50, 58).

17
Psychiatric disorders in infertile females and males The prevalence of psychiatric disorders, based on DSM-IV criteria, has been found in one study of infertile women before IVF treatment, indicating that the prevalence of major depression and generalized anxiety disorder was 17 % and 23 %, in women respectively (68). Another study compared the prevalence of psychiatric disorders in infertile subjects specifically referred or not referred to psychosomatic care and found prevalence rates of anxiety and/or depressive disorders in the latter group to be 30 % in women and 17 % in men (69). The use of a diagnostic interview to assess a psychiatric diagnosis, rather than self-report scales for depressive symptoms, is that the health profes-sional knows who is in need of specific interventions or treatment. A limita-tion with the use of self-report screening scales is that they can merely sug-gest the likelihood of a psychiatric disorder (68, 70). However, depression and anxiety have been reported more frequently by self-report scales in infertile women. Among infertile women approximately 37 % had depressive symptoms on the Beck Depression Inventory (BDI), which was twice as common as in the control group (3). According to the General Health Questionnaire, depressive symptoms were found in 33 % and 43 % of females prior to IVF and following IVF, respectively (71). Furthermore, anxiety symptoms in infertile women were encountered in 26 % of women at evaluation prior to IVF and in 22 % of women six months later using the State-Trait Anxiety Inventory (STAI) (72). Increased rates of depressive symptoms in females prior to IVF have also been reported in a recent review (73), whereas another review reported no difference in depres-sion levels between infertile females and norm groups prior to IVF (74). Few studies report on depressive and anxiety symptoms among males. The preva-lence of depressive symptoms in infertile men according to the BDI varied between 3.5 % prior to IVF and 8 % after failed IVF (75). Furthermore, anxiety symptoms in infertile men were encountered in 9 % of men at evaluation prior to IVF and in 11 % of men six months later using the STAI (72). No elevated scores for anxiety using the STAI were reported among males in another assessment prior to IVF treatment (27). The variability in prevalence rates of depressive and anxiety symptoms in infertile samples is largely determined by differences in time-points for the assessments (before, during and/or after IVF), and methodological issues such as the use of different standardized psychometric self-report instru-ments and the use of different cut-off scores (73).

18
Thus, the prevalence of psychiatric disorders, based on DSM-IV criteria, is largely unknown among unselected infertile couples undergoing IVF. To our knowledge there are no existing data about the prevalence among infertile men undergoing IVF.
Risk factors for mood and anxiety disorders A vulnerability to develop depression is suggested to depend on a previous history of depression, pre-existing stressful life events and personality fac-tors (40, 46, 47, 60). Other factors are previous reproductive failure and ge-netic predisposition (46, 47). Exposure to stressful life events is also sug-gested to be higher among subjects with a history of depression (76, 77). Risk factors for depression and anxiety in the general population include low socioeconomic status, smoking, drug and alcohol abuse, being single and being unemployed (55, 57, 78), which is fairly consistent with risk factors for psychiatric disorders in a population-based sample of Swedish pregnant women (79). Obesity is another major health concern associated with de-pressive and anxiety disorders (80, 81). However, results from a systematic review suggest that firm conclusion can not be made of the effect of obesity on depression (82). Prospective studies of risk factors for mental health in infertile females un-dergoing treatment are scarce (74). Compared to the general population, it can be assumed that other risk factors are of importance as IVF couples are by definition in stable relationships (83) and presumably avoid smoking and alcohol use to a greater extent. IVF-related factors, such as female age, dura-tion of infertility and cause of infertility have been suggested to be risk fac-tors for anxiety and/or depression in the IVF setting (28), whereas other studies show no correlation between female age, duration of infertility and depressive symptoms (3, 84). Furthermore, given the variation in emotional reactions to infertility, it is of importance to identify risk factors for adverse reactions and individuals at risk to develop depression undergoing IVF.

19
Personality traits Personality traits are an individual’s characteristic relatively lasting ways of thinking, feeling and behaving (85). Once adulthood is reached, personality traits are considered to be fairly stable over time (86-88). Personality traits related to neuroticism can be used to identify individuals at risk for devel-opment of psychiatric disorders (89). An association between neuroticism-related personality traits and major depression has been established (88, 90, 91) and according to the “vulnerability model” these traits are considered a risk factor for the development of depression (92).
Individuals with high scores of neuroticism, or negative affect, are anxious, vulnerable to stress, lack self-confidence and are easily frustrated (85, 93). The relationship between neuroticism and major depression is suggested to be the result of common genetic factors that predispose to both neuroticism and major depression (94). Furthermore, certain personality traits may affect the possibility of experiencing major life events as stressful, and stressful life events may, in turn, predispose to development of a depressive episode (95). These relationships raise the possibility that certain personality traits, such as neuroticism, could predispose to development of depression and anxiety in response to the infertility crisis and the emotional burden of IVF treatment. Studies of personality traits in relation to emotional response to IVF treat-ment are limited (30) and associations between personality traits and psychi-atric disorders in infertile females and males undergoing IVF have not been previously assessed.
Experiences of childlessness after the end of IVF Emotional reactions to infertility have been explored in women before (39, 44) and during fertility treatment (84, 96, 97). However, long-term follow-up after the end of unsuccessful IVF has not been conducted to the same extent (98-100). Grief is one of the main experiences of being childless two years after ending unsuccessful IVF (101). However, qualitative studies focus on women (101-103) or interviews have been made with the couple together (104-106). Hence, there is a need to obtain a more in-depth understanding of both men’s and women’s experiences after unsuccessful IVF treatment. The conceptual framework of crisis theory, modified for the purpose of infer-tility, was used in the qualitative-approach study (2, 39).

20
Aims
The specific aims of the following Papers were;
I. to determine the prevalence of mood and anxiety disorders in infer-
tile women and men undergoing IVF treatment
II. to identify IVF-related risk factors for mood and anxiety disorders in infertile women and men undergoing IVF treatment
III. to determine whether certain personality traits, such as neuroticism,
are associated with mood and/or anxiety disorders in infertile women and men undergoing IVF treatment
IV. to explore the experience of childlessness in infertile women and
men three years after unsuccessful IVF treatment

21
Materials and methods
Study sample papers I - III All female and male partners in consecutive couples undergoing IVF or ICSI treatment at the Centre of Reproduction, Uppsala University Hospital, Upp-sala, Sweden, were approached for participation in the study between April 2005 and April 2007.
Study setting papers I-IV In Sweden, ART is offered by public and private clinics. The Centre of Re-production is public, and infertile couples are offered three subsidised IVF treatments with a waiting list of three months at the time of the study. The upper age limit for IVF at the Centre of Reproduction is 40 years for females and 55 years for males. After the subsidised treatments are completed the couple may decide to continue privately paid treatment at the public clinic or at a private clinic. The cost for IVF treatment at the public clinic at the time of the study was about 22 000 SEK. Counselling was offered to all couples at their first visit to the clinic. Couples can seek medical care with or without referral; those who are referred from areas outside Uppsala County are pre-treated at the referring clinic. Subjects pre-treated at their home clinic visit the Centre of Reproduction for the first time on the day of oocyte retrieval. The pregnancy test (hCG in urine) is assessed at home by the female 16-19 days after oocyte retrieval.
Study design papers I-III On the day of oocyte retrieval, each eligible subject was asked for written consent to participate in the study and to individually complete and return the two questionnaires included in the study. The personality questionnaire (paper III) was included in the study a few months later (August 2005). Study exclusion criteria were (1) unable to read and understand the ques-tionnaire because of language difficulties and (2) couples undergoing cycles with gamete donation, i.e. oocyte and sperm donation. Furthermore, subjects

22
already evaluated at the time of an earlier IVF treatment during the study period were not approached to participate.
Psychiatric assessment The PRIME-MD (Primary Care Evaluation of Mental Disorders) system was developed to screen, evaluate, and diagnose psychiatric disorders according to DSM-IV criteria in primary care settings and has been validated (70, 107). Prior studies have indicated good agreement between PRIME-MD diagnoses and those of independent mental health professionals, with a sensitivity of 83 %, a specificity of 88 % and a positive predictive value of 80 % (70). Given its utility and ease of use, the PRIME-MD was considered a suitable tool for assessing the prevalence of psychiatric disorders in the IVF setting. The original PRIME-MD system (70) consists of two components: a one-page patient questionnaire (PQ), appendix I, and a 12-page clinician evalua-tion guide (CEG), which is a structured interview guide that is followed when evaluating the responses on the PQ. The CEG contains modules for mood, anxiety, eating disorders, alcohol abuse, social phobia, and obsessive-compulsive disorder. Only those modules that are indicated by the patient on the PQ are administered. A modified form of the PRIME-MD patient ques-tionnaire, containing 24 questions evaluating somatoform disorders, mood disorders, anxiety disorders and eating disorders, was used for this study. The PRIME-MD system evaluates the presence of 20 possible psychiatric diagnoses, of which this study focused on 11. Among these 11 diagnoses, eight correspond to the specific requirements of “full” DSM-IV diagnoses, such as major depressive disorder, dysthymia, partial remission of major depressive disorder, generalized anxiety disorder, panic disorder, obsessive-compulsive disorder (OCD), social phobia and bulimia nervosa, specified in appendix II (49). Three additional diagnoses are considered to be “sub-threshold” diagnoses, minor depressive disorder, anxiety not otherwise specified (NOS) and eating disorder NOS. Subthreshold diagnoses have fewer symptoms than required for a specific DSM-IV diagnosis but are in-cluded in the study as they are also associated with considerable disability, as in the case of minor depressive disorders (108). Furthermore, in this thesis questions concerning bipolar disorder, somatoform disorders and alcohol abuse were not assessed. In addition, the PRIME-MD system does not assess the distress/impairment criteria.

23
Along with the PRIME-MD patient questionnaire (PQ) the subjects were asked to provide their name, date of birth, telephone (cellphone) number, and a signed informed consent form allowing for a telephone interview (in case of positive responses on the PQ). Subjects were considered to be screen-positive if a response to any key question on the PQ indicated a psy-chiatric disorder. Screen-negative subjects were those whose responses on the PQ did not include items suggesting psychiatric symptoms. To confirm a diagnosis a telephone interview, using a highly structured computerized version of the CEG, was conducted individually with the screen-positive women and men. Prior to the interviews subjects were in-formed that additional questions would be left until after the interview. In case of a PRIME-MD diagnosis, the subject was asked about current antide-pressant drug therapy and/or psychotherapy and about previous history of depression. All subjects who fulfilled criteria for a DSM-IV diagnosis were offered referral to psychiatric specialist care. The telephone interview was conducted 21 days after screening, i.e. after the pregnancy test had been performed. At the time of the telephone interview the interviewer had no knowledge of the pregnancy test result.
Personality assessment The Swedish universities Scales of Personality (SSP) is a self-rating ques-tionnaire based on the Karolinska Personality Scales (109). Compared to KSP, the SSP has a reduced number of items and improved psychometric quality (110). The SSP contains 91 items divided into 13 scales each with seven items: Somatic Trait Anxiety, Psychic Trait Anxiety, Stress Susceptibil-ity, Lack of Assertiveness, Embitterment, Detachment, Social Desirability, Trait Irritability, Mistrust, Verbal Trait Aggression, Physical Trait Aggres-sion, Impulsiveness and Adventure Seeking (110), paper III. The participants rated the items on a scale from 1 to 4, where 1 equals ”does not apply at all” and 4 equals “applies completely”. The SSP scores were transformed into normative T-scores with means of 50 and standard devia-tions of 10 based on a representative Swedish non-patient sample, (110). The SSP scores were adjusted for age and gender (111). Sociodemographic data were collected by asking the subjects to fill in a separate questionnaire with questions on socioeconomic factors. The fertility history and outcome of IVF (pregnancy test result and live birth rate) were obtained from the subjects’ medical records after all subjects had partici-pated in the study.

24
Statistical/Data analyses papers I-III Continuous variables were compared by the use of independent t-tests and are presented as means ± SD. Frequencies were compared between groups using the chi square test. A p-value less than 0.05 was considered significant. Demographic and fertility data were compared between subjects with a psy-chiatric disorder and subjects with no psychiatric disorder; the latter group consisted of screen-negative subjects and screen-positive subjects in whom no psychiatric diagnosis was established during the telephone interview.
Statistical/Data analyses papers II-III Multiple logistic regression analysis was used to calculate adjusted odds ratios (OR) and 95 % confidence interval (CI) (112). All variables were di-chotomized and assessed in unadjusted analyses before entered into multiple logistic regression analyses. The reason for dichotomizing the variables was to obtain variables of clinical importance for IVF treatment (113). Multiple logistic regression analyses were performed with the forced entry method. In this approach all independent variables are tested in one block, not stepwise (114). Only variables with a p-value of 0.25 or less in the unadjusted analy-sis were included in the final model with any mood or any anxiety disorder as dependent variable, in paper II (113). The exception were age, smoking, duration of infertility, cause of infertility and pregnancy test result, as they are factors of clinical importance for the IVF treatment and possible risk factors in subjects undergoing IVF. Detailed descriptions of other included variables have been presented in paper II. All statistical analyses were per-formed with SPSS 15.0. A two-sided p-value less than 0.05 was considered significant. In paper III, variables with a p-value of 0.25 or less were included in the logistic regression model with any psychiatric disorder (mood and/or anxi-ety) or live birth as dependent variable. Factor analysis with varimax rotation was performed to identify factors with eigenvalues > 1. The limit for factor loading was set at > 0.45. The analysis yielded a three-factor model that was related to the personality factors neuroticism, aggressiveness and sensation-seeking (110).
Study design, participants and data analyses paper IV Women and men who had undergone IVF/ICSI treatment at the Centre of Reproduction, Uppsala University Hospital, Sweden after August 2001 par-

25
ticipated in the study. The methodological approach was qualitative with semi-structured interviews and qualitative content analysis (115, 116). Participants were identified from the database at the clinic and recruitment was in two steps. First, an invitation letter including a written consent to participate was sent to women and men who had undergone IVF (and/or frozen embryo transfer) and had no more IVF treatments at this clinic during a minimum of three years. Forty-nine letters were sent out before the de-sired sample was recruited. Second, the men and woman were contacted by phone by the first author (HV) about a week after the letter was received; this provided an opportunity for the potential participants to ask questions, to check for exclusion criteria unavailable in the database and to book a place and time for an interview. The exclusion criteria were (1) unable to understand the questions because of language difficulties, (2) having a bio-logical child from previous relationship and (3) already adopted a child. The participants were individually interviewed in the same non-clinical re-search room at the hospital. All interviews were conducted in 2006 by the first author. Prior to the interview written informed consent was obtained and socio-demographic and fertility data were collected via a questionnaire. Fertility history was obtained from the medical records. The interviews started after informing the participant that she or he could choose to end the interview at any time. In the individual semi-structured interviews a pre-tested and revised inter-view-guide covering the following topics was used; life situation as involun-tary childless, partner relationship and social network and support, mental health during and three years after IVF and decision-making when to end IVF. All interviews were tape recorded, lasted a mean of 40 minutes and then they were transcribed verbatim by the first author. The interviewer was known to some participants due to working as a midwife at the Centre of Reproduction. The interviews were analyzed by qualitative content analysis (115), by the first author and interpretations were checked against the co-authors in 2009. After careful reading the transcribed interview text was divided into meaning units. A meaning unit is a piece of text with a specific content that relates to the aim of the study. All meaning units were thereafter condensed; a process of shortening the text while still preserving the core content, into condensed meaning units. The condensed meaning units were further shortened into codes; a labeling that allows the data to be understood in relation to the con-text. Codes were then grouped into categories depending on similarities and differences in content (115).

26
Ethical considerations Women and men gave their written informed consent prior to inclusion to the studies I-IV. The study procedures were in accordance with ethical stan-dards and the Research Ethics Committee, Uppsala University, Uppsala, Sweden approved the study. All women and men who participated in the main study (I-III) and revealed a psychiatric diagnosis were offered referral to a psychiatrist. Participants in the qualitative study (IV) were offered con-tact with one of the physicians in the study if that was considered needed. The research topic, assessing the prevalence of psychiatric disorders and experiences after the end of unsuccessful IVF treatment, must be considered as one of the most sensitive topics to address in clinical research. However, participation was voluntarily and did not affect the IVF treatment for those included in the main study, as the IVF team was not told who was participat-ing or not participating. For the participants in the qualitative study the treatment had already ended. In the main study the participants could decline to participate by either not accepting or not handing in the questionnaire or by declining to participate in the following telephone interview. In the quali-tative study no reminders were used after the first telephone invitation, as the topic could be sensitive for subjects and remind them of the treatment fail-ure. The aim of the semi-structured interview was described in the covering letter. Information that the participant could choose to end the interview at any time during the interview was given.

27
Results
Prevalence of mood and anxiety disorders (paper I) A detailed description of the study population is presented in paper I. The study sample wherein a possible confirmation of a psychiatric diagnosis could be made consisted of 825 subjects (413 females and 412 males), see Figure I.
QuestionnairesFemales/males=1090
545 couples
Respons rate 80,5 %females n= 439
Respons rate 77,6%males n= 423
screening positive females n= 287
65,4%
screening positivemales n= 165
39,0%
not phoned n= 26 phone interview=261
not phoned n=11phone interview=154
Diagnosis femalesn= 127 30,8%
Diagnosis malesn=42 10,2%
screening negativefemales=152 34,6%
Attrition females= 106 Attrition males=122
screening negativemales=258 61,0%
QuestionnairesFemales/males=1090
545 couples
Response rate 80.5 %females n= 439
Response rate 77.6%males n= 423
screening positive females n= 287
65.4%
screening positivemales n= 165
39.0%
not phoned n= 26 phone interview=261
not phoned n=11phone interview=154
Diagnosis femalesn= 127 30.8%
Diagnosis malesn=42 10.2%
screening negativefemales=152 34.6%
Attrition females= 106 Attrition males=122
screening negativemales=258 61.0%
Figure I Flowchart of the study

28
Demographic and fertility data are given in paper 1 for female and male subjects included and not included in the study. The only difference was that ICSI treatment and previous IVF/ICSI were more prevalent in men who declined to participate than in men who participated in the study, p < 0.05. Demographic and fertility data are given in Table 1 for female and male subjects with or without psychiatric diagnoses. Three out of four couples were undergoing their first IVF and one in 10 cou-ples (11 %) was undergoing their third IVF. When unadjusted analyses were made between females undergoing their first IVF (n=308) and females un-dergoing subsequent IVF (n=105) no differences were found for females with or without any psychiatric disorders. Males with anxiety disorders were more often undergoing their first IVF n=11 (55 %) compared with those with previous IVF n=9 (45 %), p < 0.02, data not shown in paper I. Among subjects who filled out the PQ, 287 (65 %) women and 165 (39 %) men were screen-positive in that they triggered any of the key questions for psychiatric disorders. Of the total of 413 women in the study sample, 127 (31 %) had one or more psychiatric disorders. The corresponding figure for the 412 men was 42 (10 %). Mood disorders were the most prevalent psy-chiatric disorder and were found in 108 (26 %) females and 38 (9 %) males. Major depression, the most prevalent mood disorder, was present in 45 (11 %) women and 21 (5 %) men. Anxiety disorders were prevalent in 61 (14 %) women and 20 (5 %) men see Table 2. Of the subjects with full DSM-IV diagnoses (n = 111); 20 (18 %) subjects had received some form of psychotherapy and seven (3 women and 4 men) subjects (6 %) had been prescribed antidepressant treatment with or without psychotherapy. Forty-nine (60.5 %) of the females (n = 81) and 16 (53 %) of the males (n = 30) with full DSM-IV diagnoses reported a previous history of depression. Recurrent thoughts of death during the last two weeks were reported by 8 (18 %) females and 5 (24 %) males diagnosed with a major depression.

29
Table 1 Demographic and fertility data for infertile women and men with or without psychiatric diagnosis Female subjects
n = 413 Male subjects
n = 412 Psychiatric
diagnosis n = 127
No psychiat-ric diagnosis
n = 286
Psychiatric diagnosis
n = 42
No psychiat-ric diagnosis
n = 370 Age, years 32.7 ± 4.1 32.9 ± 3.7 35.5 ± 4.5 34.6 ± 4.8 BMI, kg/m²1 24.7 ± 4.1 23.9 ± 4.1 26.1 ± 4.4 25.5 ± 3.3 Smokers, n 10 (7.9 %) 13 (4.5 %) 4 (9.5 %) 15 (4.1 %) Snuff taking status, n
3 (2.4 %) 11 (3.8 %) 10 (23.8 %) 101 (27.4 %)
University/College, n
64 (50.4 %) 156 (54.5 %) 17 (40.5 %) 165 (44.6 %)
High school educa-tion, n
63 (49.6 %) 130 (45.5 %) 25 (59.5 %) 205 (55.4 %)
Employee/student2, n
75 (59.1 %) 165 (57.7 %) 19 (45.2 %) 222 (60.0 %)
Unemployed2, n 8 (6.3 %) 8 (2.8 %) 3 (7.1 %) 10 (2.7 %)
Duration, months 38.3 ± 20.2 38.8 ± 19.2 39.7 ± 20.6 38.0 ± 19.4
Infertility factors Female Male Unexplained Other3
41 (32.3%) 42 (33.0%) 41 (32.3%) 3 (2.4%)
81 (28.3%) 86 (30.1%) 105 (36.7%) 14 (4.9%)
8 (19.0%)
14 (33.3%) 17 (40.5%)
3 (7.1%)
115 (31.1%) 111 (30.0%) 128 (34.6%) 16 (4.3%)
Previous pregnancy No Yes
81 (63.8%) 46 (36.2%)
208 (72.7%) 78 (27.3%)
Parity Nullipara Multipara
113 (89.0%) 14 (11.0%)
261 (91.3%) 25 (8.7%)
IVF ICSI
78 (61.4%) 49 (38.6%)
175 (61.2%) 111 (38.8%)
23 (54.8%) 19 (45.2%)
233 (63.0%) 137 (37.0%)
Previous IVF/ICSI No Yes
92 (72.4%) 35 (27.6%)
215 (75.2%) 71 (24.8%)
27 (64.3%) 15 (35.7%)
285 (77.0%) 85 (33.0%)
No significant differences were found between the groups. 1 BMI = body mass index 2 missing data; a total of 157 (38.0%) females and 158 (38.3%) males. (This question was included later in the study) 3other causes or not evaluated

30
Table 2 Prevalence of psychiatric disorders detected by PRIME-MD Psychiatric disorder
Females n = 413
Males n =412
Any psychiatric diagnosis
127 (30.8 %) 42 (10.2 %)
Full DSM-IV diagnoses¹
81 (19.6%) 30 (7.3%)
Subthreshold diagnoses2
46 (11.1%) 12 (2.9%)
Any mood disorder3
108 (26.2 %)
38 (9.2 %)
Major depressive disorder
45 (10.9 %) 21 (5.1 %)
Dysthymia
6 (1.4 %) 1 (0.2 %)
Partial remission of major depressive disorder
25 (6.1 %) 8 (1.9 %)
Minor depressive disorder
35 (8.5 %) 9 (2.2 %)
Any anxiety disorder3
61 (14.8 %)
20 (4.9 %)
Anxiety NOS
46 (11.1 %) 16 (3.9 %)
Generalized anxiety disorder
7 (1.7 %) 3 (0.7 %)
Panic disorder
5 (1.2 %) 2 (0.5 %)
Obsessive-compulsive disorder
8 (1.9 %) 1 (0.2 %)
Social phobia
5 (1.2 %) 2 (0.4 %)
Eating disorder NOS
1 (0.2 %)
0
1 Full DSM-IV diagnoses; major depressive disorder, dysthymia, partial remission of major depressive disorder, generalized anxiety disorder, panic disorder, obsessive-compulsive disor-der, social phobia and bulimia nervosa 2 Subtreshold diagnoses; minor depressive disorder, anxiety NOS and eating disorder NOS 3 subjects can have one or more psychiatric diagnoses within any mood and/or any anxiety disorders

31
Risk factors for mood and anxiety disorders (paper II) The overall treatment outcome in the study population of 413 females was 136 (32.9 %) positive pregnancy tests, resulting in 100 live births (24.2 %) after treatment cycle. Fertility factors and outcome of IVF treatment for women with or without any psychiatric disorder are presented in Table 3. There were no differences in fertilization factors such as number of oocytes retrieved, fertilization rate and number of frozen embryos or treatment out-come (pregnancy test result) between females with or without any psychiat-ric disorder. Following multiple logistic regression, a negative pregnancy test and obesity (BMI � 30) were independent risk factors for depressive disorders in fe-males. Among males the only independent risk factor for depression was unexplained infertility. No IVF-related risk factors for anxiety disorders could be identified, see paper II. A negative pregnancy test, previous pregnancy and smoking were independ-ent risk factors for major depression in females (n = 45), see Table 4. Previ-ous extrauterine pregnancies had occurred in 11 % (n = 5) of females with major depression compared to 2.8 % (n=8) of females with no psychiatric diagnosis, p < 0.008. For females with major depression the live birth rate was 9 % (n = 4) compared to a live birth rate of 26 % among women with no psychiatric diagnosis (n = 74), OR 3.57; 95% CI, 1.23 - 10.32, p < 0.02.
Language difficulties were an exclusion criterion in the study. However, it was possible to include a few subjects, 24 women (6 %) and 19 men (5 %) with other ethnical background than Swedish. Therefore, the variable native language other than Swedish was used in the unadjusted analyses.

32
Table 3 Fertility factors and outcome of IVF treatment for females with or without any psychiatric disorder
Females Any psychiatric disorder
n = 127
No psychiatric diagnosis n = 286
Oocytes at oocyte retrieval (n)
11.4 ± 6.6 10.4 ± 6.0
Fertilization rate (%) 55.3 ± 27.4 55.3 ± 28.3 Embryo Transfer (ET) Yes No
115 (90.6%) 12 (9.4%)
245 (86.3%) 39 (13.7%)
Embryos at ET (n) 1.1 ± 0.5 1.0 ± 0.5 Numbers of frozen embryos after ET
2.1 ± 2.6 1.6 ± 2.4
Pregnancy test Positive Negative
35 (27.6%) 92 (72.4%)
101 (35.3%) 185 (64.7%)
Ultrasound Clinical pregnancy Biochemical Empty gestational sac
27 (21.3%)
3 (2.4%) 5 (3.9%)
88 (30.8%)
8 (2.8%) 5 (1.7%)
Miscarriages Extrauterine pregnancy Miscarriage < week 12 Miscarriage > week 12
0
1 (0.8%) 0
1 (0.3%)
12 (4.2%) 1 (0.3%)
Live birth rate Yes No
26 (20.5%) 101 (79.5%)
74 (25.9%) 212 (74.1%)
Mode of delivery Vaginal delivery Caesarean section
22 (84.6%) 4 (15.4%)
54 (73.0%) 20 (27.0%)

33
Table 4 Associations between socio-demographic, fertility data and major depression in females Major
depression females (n=45)
No psychiatric diagnosis females (n=286)
Adjusted
Odds ratio
95% Confidence
interval
Pregnancy test Positive Negative
9 (20.0%)
36 (80.0%)
101 (35.3%) 185 (64.7%)
ref
2.23*
1.01 – 4.94 Age (years) < 35 � 35
29 (64.4%) 16 (35.6%)
183 (64.0%) 103 (36.0%)
ref
0.71
0.35 – 1.45 Smoking Non-smoker Smoker
40 (88.9%) 5 (11.1%)
273 (95.5%) 13 (4.5%)
ref
3.28*
1.03 – 10.40 Previous pregnancy No Yes
24 (53.3%) 21 (46.7%)
208 (72.7%) 78 (27.3%)
ref
2.17*
1.11 – 4.25 Infertility duration (months)
< 36 � 36
31 (68.9%) 14 (31.1%)
176 (61.5%) 110 (38.5%)
ref
0.70
0.35 - 1.40 Infertility causes Male Female Unexplained
11 (24.4%) 20 (44.4%) 14 (31.1%)
86 (30.1%) 85 (29.7%) 115 (40.2%)
ref
1.77 1.02
0.77 – 4.03 0.43 – 2.41
*p < 0.05, Multiple logistic regression based on 331 subjects

34
Personality traits associated with mood and anxiety disorders (paper III)
For this sub-study 856 eligible women and men, 428 couples, were ap-proached to participate. In all 643 (75 %) subjects filled out the SSP ques-tionnaire. The response rates were 75.5 % for women (n = 323) and 75 % for men (n = 320). The overall treatment outcome in this study population of 323 women was 111 positive pregnancy tests (pregnancy rate of 34.4 %), resulting in 80 live births (live birth rate of 24.8 %). Any mood and/or anxi-ety disorder was prevalent among 100 (31 %) of the 323 women and 30 (9 %) of the 320 men. Mood disorders were present in 84 (26 %) women and in 27 (8 %) men and anxiety disorders in 53 (16 %) women and in 11 (3 %) men, due to co morbidity, data not shown. Both women and men with mood and/or anxiety disorders had higher mean scores on somatic trait anxiety, psychic trait anxiety, stress susceptibility, lack of assertiveness and embitterment compared to women and men without mood and/or anxiety disorders, see paper III. The 13 personality scales yielded a three-factor model in the factor analysis, neuroticism, aggressive-ness and sensation-seeking (extraversion). To simplify the multiple logistic regression models, these personality factors were used instead of the indi-vidual personality traits. High scores of the personality factor neuroticism and a negative pregnancy test after IVF were independently associated with mood and/or anxiety dis-orders among infertile women, see Table 5. Among men high scores of neu-roticism and unexplained or male infertility factor were independently asso-ciated with mood and/or anxiety disorders, see paper III. The final multiple regression model indicated that high scores of neuroticism were negatively associated with live birth (p < 0.04) after IVF. Live birth was also negatively associated with low scores of aggressiveness (p < 0.02), see paper III.

35
Table 5 Associations between personality traits, socio-demographic, fertility data and any psychiatric disorder in women Women
Any psychiatric
disorder (n = 100)
No psychiatric diagnosis (n = 223)
Unad-justed Odds ratio
Adjusted
Odds ratio
95.0 % Confidence
Interval
Neuroticism Low scores High scores
29 (30.5%) 66 (69.5%)
113 (51.1%) 108 (48.9%)
ref
2.38*
ref
2.21*
1.26 – 3.85 Aggressiveness Low scores High scores
42 (44.7%) 52 (55.3%)
113 (52.3%) 103 (47.7%)
ref
1.35
ref
1.09
0.63 – 1.87 Age (years) < 35 � 35
65 (65.0%) 35 (35.0%)
146 (65.5%) 77 (34.5%)
ref
1.02
ref
0.90
0.52 - 1.58 BMI (kg/m²)
< 30 � 30
87 (87.9%) 12 (12.1%)
199 (92.1%) 17 (7.9%)
ref
1.61
ref
1.65
0.73 – 3.72
Smoking Non-smoker Smoker
93 (93.0%)
7 (7.0%)
214 (96.0%)
9 (4.0%)
ref
1.79
ref
1.52
0.52 – 4.48
Previous pregnancy No Yes
64 (64.0%) 36 (36.0%)
161 (72.2%) 62 (27.8%)
ref
1.46
ref
1.28
0.73 – 2.23 Pregnancy test Positive Negative
27 (27.0%) 73 (73.0%)
84 (37.7%) 139 (62.3%)
ref
1.63
ref
1.80*
1.02 – 3.15 BMI=body mass index, * p < 0.05 Multiple logistic regression based on 303 subjects, 20 subjects had missing data.
Experiences of childlessness three years after unsuccessful IVF (paper IV) The study group consisted of 19 participants; seven were couples and two male and three female participants did not bring their partners to the study. Of the latter participants, two of the men and two of the women had partners with a biological child from a previous relationship and these partners were excluded. One female participant was divorced. The participants had their last IVF treatment at the public clinic at a mean of 38 months prior to data collection. The analyses resulted in two main categories and seven sub-categories describing the experiences of the participants.

36
Experiences in relation to IVF treatment and failure Hope turned into grief Prior to IVF both men and women described they felt optimism and hope. Unsuccessful IVF had affected mental health negatively. Grief and symp-toms of depression after IVF failure were disclosed by women. The experi-ence was described as losing someone close, and suicidal thoughts after treatment failure were revealed. Men had no knowledge of possible emo-tional reactions following unsuccessful treatment, and the grief reactions of their wives were unexpected. Not allowing oneself to grieve, ignoring the grief and continuing with the next treatment were described by men and women. Late realisation of the need for professional support A lack of professional support during IVF or following unsuccessful treat-ment was described by both men and women. Men felt that they were ex-pected to take a supportive role and they showed no sadness or grief when treatment failed. Handling their own and their partner’s grief reactions after treatment failure were experienced as difficult. Individual support and coun-selling for men was suggested, as this would enable them to ask about and better understand their spouse’s unexpected grief reactions without the spouse being present. Frustrating and unstructured ending of treatment After the last IVF treatment a final consultation with a health professional was lacking according to both men and women. Treatments were described as being too forced with too many doctors involved and the end was often abrupt. Reasons for discontinuing IVF treatment were the women’s emo-tional reactions after IVF failure, medical factors and financial factors. Men described that it had been the wife’s decision not to continue further IVF and that they were not always in agreement with their spouse about ending IVF and feelings of frustration over the decision were expressed. Affected partner relationship The partner relations had been both positively and negatively affected by IVF. Men and women described both a strengthened relationship and strain and temporary separations. A lack of self-esteem, expressed as worthless-ness, was described by women. The subject of sexuality was spontaneously mentioned during the interview by women but not by men. Sexual life had been negatively affected during IVF and for some women it was still a prob-lem three years later.

37
Experiences as childless after IVF failure Unanswered questions after ending IVF Remaining unanswered questions three years after IVF were described by both men and women. Not having the infertility factor finally explained and therefore not knowing the cause of infertility were reasons mentioned as hampering the processing of childlessness among both men and women. No fertilization after IVF was explained as a reason for understanding that the chance of treatment success was over. Feeling left out and lacking understanding Both men and women expressed a lack of understanding on the part of their closest family and friends about infertility and its treatment. Another reason for a lack of understanding was that men and women had provided informa-tion and was communicated about their fertility problems differently. Having social support was not described as often among men as by women. Men described feeling excluded in social situations when friends and colleagues were talking about their children. Experiences of not being like others, not being able to have children, and not being able to create a family were de-scribed by the women. Meaning of life affected Adaptation to childlessness had not been reached three years after IVF. Men described how they were trying to learn to live with the pain by denying it. Women described how they was physically and rationally close to accepting childlessness however there would never be an emotional acceptance. Three years after ending IVF mental health was described as relatively stable among men. Women were more emotionally stable than during IVF but some still had symptoms of depression. Not knowing how to handle and process grief was revealed. Feelings of guilt were described by women, but not by men, and a loss of control of the situation as childless. The loss of parenthood, of not having a family including a child, was described as a different life situation. At the same time, a life with more freedom was de-scribed. Still having hope for a spontaneous pregnancy was expressed among women, but also how their hope for a child had taken up a great deal of time in their life. The future was described in thoughts of being alone in old age. Both men and women described disappointment of not being able to give their parents the joy of grandchildren and not being able to have their own grandchildren.

38
Discussion
Methodological considerations papers I-III Psychiatric disorders were assessed by the use of the PRIME-MD screening questionnaire followed by a highly structured interview conducted by tele-phone. Diagnostic interviews can also be conducted by semi-structured in-terviews, such as the SCID (Structured clinical interview for DSM-V disor-ders), with more open-ended questions for psychiatric assessments. A limita-tion of the PRIME-MD is that questions concerning distress/impairment are not assessed. The use of the clinician evaluation guide (CEG) in PRIME-MD by a tele-phone interview has been validated in comparison with face-to-face inter-views conducted by primary care physicians with good agreement (70, 107, 117). Telephone interviews are commonly used in large-scale population-based studies of psychiatric disorders because of their demonstrated compa-rability with face-to-face research interviews (70, 118, 119). For this reason, and because approximately 40 % of the subjects were living outside of Upp-sala County, the structured computer-based interview by telephone was used for the psychiatric assessments in this study. The choice of time-points for the assessment of psychiatric disorders may be considered as a limitation of the study. We chose a time-point for the final evaluation (CEG) which we thought would be most relevant to the couples undergoing IVF, i.e. after the pregnancy test result. A number of considera-tions were taken into account when this decision was finalized. First, a base-line assessment at the start of the infertility evaluation or at the onset of IVF treatment was discussed. From a clinical perspective this would have been a valuable time-point as we then would have been able to assess which sub-jects were depressed already at onset of IVF and in need of specific interven-tions during the course of treatment. However, almost half of the couples were referred from other counties, and by the time they first came to the Centre of Reproduction infertility evaluation and pre-treatment for IVF had been initiated by the referring clinic. With such a design, we would have ended up having a smaller sample or extending the inclusion period substan-tially.

39
Furthermore, whether this time-point would have resulted in a more valid estimate of the prevalence rates for depression and/or anxiety is uncertain. Increased rates of depressive symptoms in females prior to IVF have been reported in a review by Williams and co-authors (73), whereas a review by Verhaak and co-authors reported no significant difference in depression lev-els between infertile females and norm groups prior to IVF (74). Also, it has been shown that women express unrealistically high expectations when treatment is initiated, which may underestimate the clinical problem (27-30). Another time-point that was discussed was whether the initial screening (PQ) should be performed on the day of oocyte retrieval or on the day of embryo transfer. In order to increase the sensitivity of our assessments we chose the day of the oocyte retrieval, which is considered as more stressful than the ET procedure. In doing so, we presumably had to perform more telephone interviews with screen positive women but there is little or no evidence that this difference in time-points (two to three days in between procedures) would have had any real relevance for our outcome measures. However, by screening before treatment outcome was known to the couple we have no knowledge if there were any of the screening negative women or men that could have developed a depression. The time-point chosen for the telephone interview was after the pregnancy test had been performed. We considered performing the telephone interview prior to the pregnancy test, but this idea was rejected as this period has been shown to be the most stressful during the course of IVF (29). As the purpose of the study was to describe the prevalence rates of depression and anxiety during IVF we decided that the best time-point for the final evaluation would be after the treatment outcome was known to the couple. It is also important to stress that more than 25 % of women with depression and/or anxiety had a positive pregnancy test. A further limitation of the study was the time-point for the assessment of personality traits. Personality assessment at an earlier time-point in life, be-fore the first onset of depression (120) or before the infertility crisis started, would have been preferable, although this was not feasible. Personality traits related to neuroticism are considered to be associated with major depression, although it is still debated as to whether neuroticism actually predispose to development of depression or are the result of one or several depressive epi-sodes (120, 121). Another methodological consideration was that alcohol abuse was not as-sessed in the modified version used for this study, even though this question was initially included in the PRIME-MD. Couples who are attempting a pregnancy are generally presumed to abstain from alcohol but the alcohol-

40
related questions could nevertheless have been of value for the study. Among men in the general population, high rates of substance-related disor-ders such as alcohol abuse, that disguise a depression have previously been reported (52, 122). Furthermore, in one study assessing alcohol abuse in primary care by the PRIME-MD the prevalence of alcohol abuse or depend-ence was estimated to 19 % in men to compare with 4 % for women (123). Most women and men with language difficulties were excluded from the study. Although a few were included (5 %), the rate of subjects with other native language than Swedish in the general population is about 16 % (8). The exclusion of individuals with other native languages is a problem in most studies where data are collected by questionnaires and interviews. It can be assumed that these individuals more often suffer from depression, as heightened depression scores have been reported previously (124). Furthermore, a variable of importance when analysing risk factors for psy-chiatric disorders is a history of depression. A previous history of depression was reported by every second subject with full DSM-IV diagnoses (paper I). However, a history of depression was only reported by females and males who received a psychiatric diagnosis during the telephone interview, and not by any other subjects included in the study. This information could have been assessed by including the question in the demographic questionnaire given to all participants in the study. For this reason prior depressive epi-sodes could not be used in the multiple logistic regression model. Similarly, the number of previous stressful life events, except for the negative repro-ductive events, was not documented in this study. However, risk factors for development of depression and anxiety are fairly well-known from previous studies and the current study aimed at evaluating possible IVF-related risk factors for depression and anxiety. It can also be argued that at a control or comparison group would have been of value in interpreting the study. However, the aim of the study was not to investigate whether IVF couples suffer more from depression and/or anxiety in comparison with other fertile women or the general population, but rather to describe the extent of this clinical problem within the IVF setting. How-ever, in comparison with previously conducted population-based studies (52, 53), mood disorders were more common among infertile couples, whereas prevalence rates of anxiety disorders were similar or even lower than in the general population. Prevalence rates of psychiatric disorders among infertile females were similar to what was found in unselected gynaecological outpa-tients (125). Likewise, compared to a population-based study of pregnant women, the prevalence rates of depression and/or anxiety disorder were higher in the infertile females (126).

41
However, strengths of the present study include the relatively large sample size for an infertility/IVF setting, and the inclusion of male subjects, the high response rate and the possibility of obtaining follow-up data on pregnancy outcomes in all subjects. Furthermore, because medical records were kept on all eligible subjects, separate analyses could be performed among subjects who declined to participate.
Methodological considerations Paper IV A qualitative approach was used for paper IV to complement the main study. A qualitative method can be used to reach a in-depth understanding of a given topic by describing in words and not in numbers, and by not explain-ing or analyzing differences in the sample (127, 128). A qualitative approach makes it possible to retrieve those answers that might be hard to assess from a quantitative study conducted by collecting data from questionnaires. One concern with assessment by questionnaires is that self-report measures may be susceptible to social desirability bias, as infertile couples want to present as well-adjusted emotionally especially prior to IVF. Participants are sug-gested to respond more as expected or more positively in questionnaires than in interviews (129, 130). Thus, open-ended interviews have a potential for a more in-depth understanding of the participant’s experiences. Validity and reliability in qualitative studies is described by credibility, de-pendability and transferability to reach trustworthiness (115). Credibility depends on the sampling and the interpretation of the collected data accord-ing to the given topic (131) and refers to the similarities within and differ-ences between categories (115), by using citations from different participants in the interviews. Another way is to test for inter-rater reliability, to avoid bias when interpreting. Thus, the co-authors checked the achieved codes and categories to reach an agreement and in this manner the interpretation was also checked for. Another way to reach inter-rater reliability can be to ran-domly choose a sample of interviews to be separately coded by the co-authors. By using qualitative content analysis the results can be described in terms of both manifest (explicit) and latent (implicit) content, which was the case in this study. This study mainly focused on the manifest content in the interviews. However, the underlying meanings, thus addressing the latent content, were also described as in the case of men not explicit expressing grief. Dependability is the possible change over time in data collection and analy-sis and if different answers are given to different interviewers (115, 116). All interviews in this study were conducted and transcribed during the same year (2006) by the same person. The interviews were assessed by an interview

42
guide to maintain the same questions to all participants, and a structured analysis including discussion among the researchers minimized the change over time. All transcribed interviews were re-checked by listening to the tapes on several occasions. The description of bias and being compliant to-wards the collected data and transcribing verbatim are of importance (116, 131). Limitations of qualitative studies are often the relatively small sample size, thus making transferability, such as to generalizing results to other settings less possible. Therefore, the extent of the transferability of the result of a study to other infertility settings depends on cultural and traditional similari-ties or differences (116). However, qualitative research does not aim at being representative in sampling, but at reaching meaning and understanding of each individual’s experience (128, 132). The experiences of individuals with ethnic backgrounds other than Swedish were not included nor were certain characteristics occurred of those declining to participate. Further, men with a male infertility factor and women with university level education who were fewer in number than in our previous infertility sample at the same clinic. Another limitation of the study was that sexual problems that some women brought up spontaneously were not a topic guiding the interviews, and thus there is no knowledge of male participants’ experiences of sexuality. However, strengths of the qualitative study, was to assess the individual male perspective after the end of unsuccessful IVF treatment, as this pro-vides new knowledge in the infertility/IVF setting. Also, to combine the main study with a qualitative method may increase the understanding of the experience of childlessness after unsuccessful IVF treatment.

43
Main outcome findings The main study (papers I-III) is to our knowledge the first to describe preva-lence, IVF-related risk factors and personality traits and associations with depressive and/or anxiety disorders in both women and men undergoing IVF treatment.
Mood disorders are more prevalent than anxiety disorders Mood disorders were common in both women and men undergoing IVF. Major depression was the most common mood disorder, prevalent in one of 10 women and twice as common as in men. However, anxiety disorders were less common than in the general population. The relatively high preva-lence rates of mood disorders may reflect the fact that the studied population was a clinical sample. Prevalence rates of psychiatric disorders among infer-tile females were similar to what was found in unselected gynaecological outpatients, where 30.5 % suffered from any psychiatric disorder and 10 % had a major depression (125). However, the prevalence of mood disorders is even higher in the primary care setting; 35 % in women and 25 % in men assessed by the PRIME-MD (123). The prevalence rates of depression and anxiety disorders can also be affected by the difficulties involved in dealing with infertility and/or the emotional burden of undergoing IVF treatment. The hormone therapy used during IVF may also affect the self-reported symptoms such as mood, headache and fatigue at the time of the initial screening. However, three out of four women in this study were undergoing their first IVF and according to de Klerk and co-workers no difference in self-reported symptoms of depression were de-tected after the first IVF treatment or between different treatment regimens (26). The majority of subjects with depressive disorders were undiagnosed. One plausible explanation for why depression is not recognized in the infertility setting is that infertile couples are reluctant to report depressive symptoms to the IVF team as they want to appear well adjusted, in concern that IVF treatment will be postponed if psychological problems are revealed (28, 73). Therefore, their positive attitudes before the start of the first treatment may disguise an ongoing depression. Another finding was that only a small proportion of those identified with mood or anxiety disorders had ongoing treatment. Only a few women with a psychiatric disorder had antidepressant treatment during the IVF treatment, although the current recommendations are not to avoid antidepressants dur-ing pregnancy (63, 64). Psychotherapy, in the form of counselling, was re-

44
ceived by only one fifth of the subjects with a psychiatric diagnosis and by one in 10 of all subjects in this study. This is surprisingly few, as all couples are informed about and offered counselling at their initial visit to the clinic. However, similar low rates of counselling have previously been reported by Boivin and colleagues, who found that only 11 % of females and males re-ceived counselling (133). Counselling is suggested according to ESHRE to be offered to all couples considering medical, psychological and social ques-tions, as an integral part of the IVF programme and may be performed by health professionals in the IVF team or by professional counsellors (12, 25). Another alternative explored is an intervention by extended encounters with a midwife during IVF treatment, however no impact was noticed on psycho-logical well-being (134). Furthermore, a recent meta-analysis examining psychological interventions for infertile women found no significant effects in mental health (135). Therefore, for those individuals at risk to develop depression psychological/psychiatric consultants and adequate evidence based treatment need to be provided.
IVF-related risk factors for mood disorders A negative pregnancy test after IVF treatment was associated with an in-creased risk of mood disorders among women, in particular major depres-sion. As the pregnancy test is taken at home by the female, a negative test result will be revealed to the couple outside the fertility clinic. Therefore, it is clinically important to follow couples after treatment failure. Infertile cou-ples need to be informed at an early time point prior to IVF that the outcome after treatment can be unsuccessful and of the emotional reactions that may follow (74). A mandatory appointment for follow-up booked prior to IVF is therefore strongly recommended. In case of treatment failure the follow-up visit at the clinic should take place within a few weeks after the negative pregnancy test. Not only is unsuccessful treatment associated with increased risk of depression, a failed treatment may lead to an increase in pre-existing depressive symptoms, which are unlikely to diminish shortly after treatment. An unsuccessful first treatment is a less favourable starting point for the next treatment cycle and may be a risk for later development of depression (74, 136). Therefore, to identify females with depression and to assure that ade-quate evidence based treatment is initiated before the next treatment is of importance. Previous pregnancy was, beside a negative pregnancy test, a risk factor for major depression in females. The prevalence of early miscarriages is be-tween 10 - 20 %. The knowledge of the prevalence of spontaneous abortions in relation to any underlying depression is limited. It is still unknown whether depression with or without treatment with antidepressants is associ-ated with spontaneous abortions (137 - 138). However, having recurrent

45
miscarriages and extrauterine pregnancies may lead to depression. Therefore, the IVF team needs to be aware of and identify those women with previous negative reproductive events, such as miscarriages or extrauterine pregnancies, as these women are particularly vulnerable to develop major depression after unsuccessful IVF treatment. Obesity (BMI � 30) was another independent risk factor associated with mood disorders in females. The prevalence of obesity in the population is increasing and it is likely that obesity and depression may occur together (139). However, no firm conclusion can be made of the effect of obesity on depression (82). Obesity may negatively affect the live birth rate after IVF and weight reduction before the onset of IVF has been shown to improve treatment outcome (13, 140, 141). Information about the negative effects of obesity is important and many clinics recommend weight reduction and have limits for BMI prior to IVF. Unexplained infertility was the only independent risk factor for depression among males. Not having an infertility diagnosis is suggested to be a stress-ful factor (142) and has to be taken into account in men undergoing IVF. Previous studies have indicated that an unexplained infertility factor can be a risk factor for distress in women (105, 143). Explaining the infertility diag-nosis may increase the sense of control (43) and decrease the risk of devel-oping depression. Today when the waiting time for infertility evaluation and treatment is shorter than a decade ago (104) and visits to the clinic are few, there is less time and opportunity for explaining the cause of infertility prior to or during IVF. Therefore, the infertility factor need to be explained not only undergoing IVF but also at a final consultation after IVF treatment. Surprisingly, fertility factors such as female age, duration of infertility, infer-tility diagnosis and number of previous IVF treatments were not associated with psychiatric disorders, although these findings are consistent with other studies (3, 84).
Personality related to mood and/or anxiety disorders High scores of personality traits related to neuroticism were independently associated with mood and/or anxiety disorders in women. Our results are in line with findings of Verhaak and co-workers, thus suggesting that pre-existing neuroticism in women are one of the most important predictors of the emotional response after IVF failure (30). High scores of neuroticism were also independently associated with mood and/or anxiety disorders among men. However, as these disorders were less prevalent among men the results in this group must be interpreted with caution.

46
Certain personality traits may increase the probability of experiencing life events as stressful (95). Infertility and treatment failure, independently or taken together qualify as stressful life events. Consequently, not only may women with high scores of personality traits related to neuroticism be more likely to perceive unsuccessful IVF treatment as more stressful than women without such an underlying predisposition, but they may also be more vul-nerable developing a depressive episode during or after unsuccessful IVF treatment. An increased awareness of these vulnerability factors for developing depres-sion is of importance for health professionals in care of infertile couples. Although personality is considered to be fairly stable and resistant to change, implications for intervention may be useful, as to modify the high expecta-tions of a positive treatment outcome and to reduce depression after treat-ment failure (144). Therefore, there is a need for a specialized IVF-team able to identify subjects at risk of depression and to provide evidence based treatment after treatment failure or before undergoing further IVF treatment.
Mood disorders and personality in relation to treatment outcome Some of the results derived from paper II and III need to be further ad-dressed, although they must be regarded as preliminary. The live birth rate (9 %) for females with major depression was significantly lower than for other females in this study population (approximately 25 %) in women with-out psychiatric diagnoses. However, in spite of the relatively small sample of women with major depression (n = 45) these findings may suggest that ma-jor depression is associated with negative outcome of IVF treatment. A re-view of the literature indicates that mood disorders may be associated with decreased pregnancy rates (73), although there is great controversy in this area. An association between anxiety and/or depressive symptoms and lower pregnancy rates has been suggested (28, 145-147), whereas other studies have failed to reveal any associations (27, 148-150). Few studies have ad-dressed the association between anxiety and/or depressive symptoms and live birth rate as endpoint. In a study by Klonoff-Cohen and co-workers live birth rate was negatively influenced by baseline stress prior to IVF (21), but this was not the case in another study by de Klerk and co-workers (151). The association between personality factors, such as neuroticism, and treat-ment outcome following IVF was explored in paper III. In contrast to paper II, the assessment of personality traits were made at the time-point of oocyte retrieval, and consequently before the result of the pregnancy test was known to the subject. The results indicate that high scores of neuroticism are negatively associated with live birth after IVF. Successful outcome after IVF depends on multiple factors such as female age and good quality embryos

47
(9, 10). According to our results, neuroticism as a vulnerability factor for depression may also be associated to treatment outcome after IVF.
Unresolved grief after IVF failure Grief and symptoms of depression were described by women both after IVF failure and three years after the end of IVF in paper IV. If the grieving proc-ess is hampered or prolonged, it may lead to complicated grief which is con-sistent with the definition of major depression (2, 47). Major depression includes feelings of worthlessness, such as loss of self-esteem which is con-trary to normal grief reactions where self-esteem is not affected (46). Feelings of guilt and lost control and suicidal thoughts after IVF failure were described among women indicating symptoms of depression. Guilt and sense of loss of control is considered a vulnerability factor for distress after IVF (28, 96). Another study revealed that a substantial proportion of childless women had high scores of complicated grief and depressive symptoms when fertility treatment was no longer an option (152). Furthermore, unresolved grief can lead to substantial disability and impairment, increased health ser-vice use and sick leave, although those questions were not assessed in this study. Therefore, it is important for health care professionals to distinguish between normal grief and complicated grief (47, 48) and to identify and fol-low the individuals at risk of developing major depression after treatment failure. Furthermore, informing and counselling about emotional reactions of grief and depression after IVF failure already at an early phase prior to IVF may help the individual in the grief process of childlessness after IVF treat-ment. Social support is depending on if there has been information given about the fertility problems, as there is no visible loss. Therefore, it is plausible that infertile individuals will be more vulnerable to depression if there is a lack of support (40, 152). If the loss is visible, as after a stillbirth, the social network will be supportive and thus facilitate an adjustment process. Social isolation, as feelings of being excluded with no understanding from their social net-work, was described mostly by men. Men and women were communicating differently about fertility problems with significant others, resulting in less social support among men. A lack of social support or discontent with sup-port given leads to complicated grief and depression in women (48, 152). A study of parents of preterm infants indicates those who actively seek social support and express negative feelings have healthier mental health outcome than those who deny negative feelings and do not seek or accept support from their social network (40). A lack of professional support and how men took the supportive role after treatment failure were also described and indi-cated men asked for and were in need of their own individual support while

48
undergoing IVF treatment. This raised the question of, if and when, will men grieve or realise they need an opportunity to grieve.
A consequence of the emotional reactions after IVF failure was to discon-tinue IVF treatment. The decision-making to end treatment was described by the men as being the woman’s decision, and one reason for this was the grief reactions experienced after treatment failure. The most common reason for discontinuing treatment is emotional burden after IVF failure (153, 154). Hence, to limit drop-out from further treatment mandatory professional sup-port should be offered all couples after treatment failure. If symptoms of depression can be identified and adequately treated, the chance may be that more couples continue and may optimise the chance of successful outcome after treatment (154). Lack of a structured end after IVF treatment is a plausible factor to hamper the processing of childlessness. Furthermore, the cause of infertility could be explained at a final consultation, thus reducing the number of unresolved questions after treatment (100). However, there are no rituals in the experi-ence of ongoing childlessness for facilitating an adaptation (39, 42, 44, 155). Achieving closure, having some kind of ending, is of importance for being able to process childlessness. Ending treatment means closure of options for having a biological child and giving up hope of pregnancy. However, the cessation of treatment does not end infertility for women, as there is no emo-tional closure, indicating an increased vulnerability to develop depression (156). The theoretical framework of life crisis was not applicable for all phases during an infertility crisis, as most men and women were still processing and had not adapted to childlessness three years after IVF treatment. Infertility differs from life crisis by an extended reactive phase resulting in a state of prolonged or chronic crisis (43). A crisis model for infertility has implica-tions for understanding the emotional adjustment of the grief process and can be of use for successful adjustment (4). However, as infertility is not a single stressful event but a complex process, often with recurrent reproductive losses (156) the crisis model may not be as useful. Crises are considered time-limited and for many individuals infertility is not limited in time be-cause of recurrent losses. Differentiating between the emotional reactions, such as stress, crisis and grief and psychiatric disorders as major depression can be difficult. Further-more, there is no clear definition of the psychological problems associated with infertility (135). For a childless woman the loss is an ongoing stressful life event, first the loss of fertility and then the loss after undergoing failed treatment when childlessness will be considered as definite. Thus, the crisis

49
can constitute lifelong grief with the risk of developing depression. Not only is infertility a reproductive health problem it may also lead to mental health problems, as major depression. IVF failure was affecting women and men differently, by women experiencing grief and men were not expressing grief. Most infertile individuals will adjust to infertility and IVF failure. However, some of the individuals with previous negative reproductive events and neu-roticism-related personality traits will be more vulnerable to develop depres-sion.
Identify risk factors Screening women and men prior to IVF to identify individuals vulnerable to develop depression may be possible by assessing the risk factors found in this study; such as previous miscarriage, obesity and the infertility factor among men. A medical and psycho-social history at the time of admission to IVF should therefore include assessment of risk factors and also a history of depression and social network/support. Although assisted treatment has developed during the last two decades, little has improved in terms of support and counselling for couples undergoing IVF, a situation described by Schmidt already a decade ago (104). Some of the suggestions given by men in paper IV included individual and mandatory support before and after IVF, an introduction prior to IVF and a treatment-plan to follow during IVF. Patient education and information for infertile couples undergoing treatment is in need of improvement (157). Therefore, these suggestions are clinical implications that are possible for the IVF team to assess for all couples undergoing IVF. These improvements are needed to facilitate the grieving process after undergoing unsuccessful IVF treatment. Furthermore, for those individuals at risk to develop depression psychologi-cal/psychiatric consultants and evidence based treatment is the option.

50
Conclusions
Mood disorders were common in both women and men undergoing IVF. Major depression was prevalent in one of 10 women and twice as common as in men. The majority of subjects with psychiatric disorders were undiag-nosed and untreated. Anxiety disorders were less common than in the gen-eral population and no IVF-related risk factors were identified. A negative pregnancy test was associated with an increased risk for depres-sion in women, whereas the pregnancy test result was not a risk factor for depression in men. An unexplained infertility factor was the only risk factor for mood disorders in men. High scores of personality traits related to neu-roticism were associated with any mood and/or anxiety disorders among both women and men. Unsuccessful IVF was experienced by women, in the qualitative-approach study, in terms of grief whereas men took upon themselves a supportive role and did not express grief. Professional support and counselling in how to handle the grief was requested. An unstructured end after IVF treatment left unanswered questions. Three years after the end of treatment, both men and women were still processing and had not adapted to being childless, indicat-ing the grieving process was unresolved.

51
Clinical implications
A midwifery perspective A midwife within reproductive health meets women during different transi-tions in a woman’s life; from the adolescent girl reaching puberty, the preg-nant woman before, during and after childbirth to the menopausal woman at the end of her reproductive life. A midwife will also meet the couple when it is not possible to reach one of these transitions, or life goals, when fertility treatment does not result in the birth of a child. At this time point it is impor-tant to be aware of the mental strain, of grief and depression that can occur. Not only reproductive health is affected, mental health may be affected as well. Therefore, involuntary childlessness, as the inability to transition from pregnancy to childbirth and parenthood is to be considered as one of the most stressful events in a woman’s life. With this knowledge and awareness in mind reproductive health profession-als, such as the midwife, can meet the couple prior to their first IVF. By ask-ing questions about previous negative reproductive events and history of depression it may be possible to identify those individuals vulnerable to de-velop depression. By also using the suggestions given by men in this study, such as providing additional individual support before IVF including infor-mation about possible emotional reactions and how to handle them after IVF failure, it may be possible to facilitate the grieving process after IVF failure. Furthermore, these clinical implications can also be used to try to limit drop-out from further IVF so that more couples will continue, thereby optimizing the chance of successful outcome after treatment. Patient information and education are important not only for the infertile couple prior to and during IVF. Information to the general population is of importance to obtain in-creased understanding of the difficulties involved during infertility and IVF treatment. Therefore, psychiatric education for health professionals in the IVF team in care of the infertile couple is of importance.

52
Future research
Clinical research often aims at describing prevalence and causes/risk factors for a given problem for those individuals requesting treatment. Thus, there is no knowledge in this respect regarding those not requesting treatment. When the result is assessed and there is a problem or risk factor revealed, one need to start addressing the problem through implementation, not only by identi-fying and recommending. Support and counselling, concerning grief reac-tions following unsuccessful treatment, by a specialized midwife in the IVF-team during and after IVF offered to all couples to decrease the mental bur-den of treatment failure and ongoing childlessness is an intervention of fur-ther research. Furthermore, there have been few long-term follow-up studies after the end of IVF treatment and no study thus far has addressed the prevalence of psy-chiatric disorders following IVF failure. Clearly, grief is a common finding in women three years after failed IVF, but our qualitative study was not de-signed to address whether these women suffered from an unresolved infertil-ity crisis, complicated grief or even major depression. The women and men who participated in studies I-III started their first (in most cases) IVF treat-ment almost five years ago and may thus be targeted for a long-term follow-up study focusing on prevalence of major depression. Possible questions to address include whether there is a difference in the prevalence rates of de-pression between women who have conceived and women who are still childless. Also, it would be possible to assess why couples discontinue IVF when treatment outcome is unsuccessful and to establish the reasons for drop-out from further IVF in a larger sample. Another issue that was brought up by women in paper IV was the negative effect infertility and IVF treat-ment had had on their sexual life. Further studies in both women and men concerning sexuality are warranted. Another topic for future research would be to describe the resolution of childlessness, such as plans for adoption, which was not assessed in the cur-rent study. Will biological childlessness result in a resolution of the infertil-ity crisis and if so how is it solved; by adoption or other alternatives? Devel-opment of a theoretical explanation-model for the infertility crisis in order to improve the understanding of involuntary childlessness is a topic that could be of use for future research.

53
Summary in Swedish – svensk sammanfattning
Infertilitet och att genomgå behandling med in vitro fertilisering (IVF) kan vara förenat med psykisk ohälsa, som depression. Egentlig depression kan fastställas med psykiatriska diagnoskriterier enligt DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition). Personlighetsdrag relaterade till neuroticism kan öka sårbarheten att utveckla depression. Syftet med detta avhandlingsarbete var att fastställa förekomsten av depres-sions- och ångestsyndrom, hos ofrivilligt barnlösa kvinnor och män som genomgår IVF behandling. Syftet var också att undersöka vilka riskfaktorer och personlighetsdrag som är relaterade till depressions- och ångestsyndrom. Ett ytterligare syfte var att intervjua kvinnor och män för att ta reda på deras upplevelse av barnlöshet tre år efter avslutad IVF. Studien genomfördes på Reproduktionscentrum, Akademiska sjukhuset, Uppsala under en tvåårsperiod mellan 2005 – 2007 där samtliga kvinnor och män (545 par) erbjöds att delta. Svarsfrekvensen var totalt 79 % (413 kvin-nor och 412 män). Två frågeformulär ingick i studien; PRIME-MD (The Primary Care Evaluation of Mental Disorders) ett psykiatriskt diagnostiskt instrument bestående av två delar; ett screeningformulär med 24 frågor, samt en uppföljande intervju som i denna studie genomfördes per telefon med screeningpositiva kvinnor (65 %) respektive män (39 %). Screening skedde i samband med äggaspiration (OPU) och följdes upp med en individuell hög-strukturerad diagnostisk telefonintervju tre veckor senare, efter graviditets-testen. SSP (The Swedish universities Scales of Personality) ett personlig-hetsformulär med 91 frågor som användes för att undersöka personlighets-drag. Resultatet från undersökningen visade att förekomsten av depression och/eller ångestsyndrom var 31 % bland kvinnor och 10 % bland män. Van-ligast förekommande var egentlig depression som diagnostiserades hos 11 % kvinnor och 5 % män. Ångestsyndrom var inte mer vanligt bland infertila kvinnor och män än i normalbefolkningen. Riskfaktorer för depression hos kvinnor var ett negativt graviditetstest efter IVF samt fetma (body mass in-dex � 30). Oförklarad barnlöshetsfaktor var den enda riskfaktorn för depres-

54
sion hos män. Inga IVF-relaterade riskfaktorer för ångestsyndrom påvisades hos kvinnor eller män. Personlighetsdrag relaterade till neuroticism var asso-cierat med depression och/eller ångestsyndrom. Intervjustudien genomfördes med kvalitativ ansats bland 10 kvinnor och 9 män, tre år efter avslutad IVF behandling. Intervjuerna genomfördes indivi-duellt, spelades in på band och nedskrevs ordagrant. Intervjudata analysera-des med hjälp av kvalitativ innehållsanalys. Resultatet visade att kvinnor uttryckte sorg och symtom som kan förekomma vid depression, efter miss-lyckad IVF behandling medan män intog en stöttande roll och uttalade inte sorg. Män beskrev att de saknade individuellt stöd för att enskilt kunna prata om de oväntade sorgereaktioner deras respektive visade efter misslyckad IVF. Både män och kvinnor saknade stöd och råd om hur de skulle bearbeta sorgen. Förhållandet till partnern påverkades både positivt och negativt av att genomgå IVF. En upplevelse av utanförskap och avsaknad av socialt stöd framkom framför allt hos män. Både kvinnor och män saknade ett sista avlu-tande samtal efter IVF. De flesta män och kvinnor hade inte bearbetat barn-lösheten tre år efter avslutad IVF behandling, vilket indikerade att sorgepro-cessen ännu var obearbetad. Avhandlingsarbetet har visat behov på ökad kunskap och förståelse om risk och sårbarhetsfaktorer för depression i samband med infertilitet och miss-lyckad IVF behandling. Det finns ett behov av utbildning inom psykiatri och psykisk ohälsa, för att öka kunskapen om bemötandet av individer i psykisk kris. Barnmorskan inom reproduktiv hälsa möter kvinnor i viktiga vänd-punkter i livet; från tonårsflickan i puberteten, kvinnan i samband med gra-viditet och barnafödande fram till den fertila periodens slut, menopaus. Barnmorskan möter också det infertila paret, som inte uppnår sitt livsmål - att få barn efter genomgången IVF behandling. Kliniska implikationer för IVF-teamet, exempelvis en specialiserad barn-morska, är att i samband med inskrivningssamtalet inför IVF ställa frågor om riskfaktorer, som i denna studie var tidigare missfall, samt om tidigare depression, för att underlätta identifiering av personer som kan ha en ökad risk att utveckla depression efter misslyckad IVF behandling. För dessa indi-vider som tidigare varit deprimerade bör psykiaterkonsult samt evidensbase-rad behandling erbjudas. Betydelsen av kontinuitet, samt ett avslutande sam-tal efter IVF framkom i studien och vikten av att informera om orsaken till barnlösheten. Andra implikationer för att underlätta bearbetande av barnlös-heten är att erbjuda stöd och råd, både individuellt och för paret, redan i ett tidigt skede av IVF om de emotionella reaktioner och den sorgeprocess som kan uppstå efter att ha genomgått misslyckad IVF behandling.

55
Förslag på framtida forskning är en långtidsuppföljning av de par i studien som påbörjade IVF behandlingen för närmare fem år sedan. Syftet är att ta reda på förekomsten av psykisk ohälsa beroende på utfallet efter IVF, dvs. om paren fått barn eller inte. Dessutom kan orsaker till att avsluta misslyck-ad IVF behandling i förtid undersökas. Frågor som inte tagits upp i denna studie; som alkoholvanor, sexualitet samt tidigare depression kan ställas. Ett annat forskningsområde är att beskriva om och hur kvinnor och män har bearbetat barnlöshetskrisen; genom adoption eller andra alternativ. Utveck-lande av en teoretisk förklaringsmodell för barnlöshetskrisen kan vara ett sätt att öka kunskapen om och förståelsen för de barnlösa parens livssituation.

56
Acknowledgements
This thesis has been made possible by many people. First I want to thank all females and males who participated in the studies. I also wish to express my gratitude to all those who have been supportive during my PhD studies. I particularly want to thank the following persons; My three supervisors; Inger Sundström Poromaa - for accepting to be my supervisor, for showing your enthusiasm and the great joy of research when sharing your knowledge in the statistical field - analyzing logistic regression can be fun - and for your skilful English writing Lisa Ekselius - for your invaluable support and the time you have dedicated sharing your knowledge in the field of psychiatry and genuine scientific skills and for instructive discussions at your room introducing me into re-search education Agneta Skoog Svanberg - for giving me the fantastic opportunity to be one of the teachers starting the first Midwifery education in Uppsala (2007) - an incredible journey beside my research - taking part of your enthusiasm and great generosity at the supervisor-meetings with dinners in your home and in the boathouse! Pia Olsson - for your co-authorship and sharing your deep knowledge and understanding in the qualitative field and for your support when analyzing interview data felt like a mountain to climb! Örjan Lundkvist - for your co-authorship – your knowledge and experience in the IVF-field is outstanding - being one of the pioneers in IVF in Sweden! Thank you for your support and for always being there even when times were tough for you and for being supportive, not only for me, as I know you are towards your patients Niklas Simberg - for actually being the first one introducing me into research within the infertility-field – by suggesting me to evaluate the couples under-going infertility work-up and by that caught my interest of the research topic

57
Ove Axelsson - for introducing me into the academic world, when I wanted to teach, by making me realize the value of scientific qualifications Lena Moby - for putting up with me as room mate and sharing all the serious and happy moments in life! All staff at the research-lab/research group - Matts Olovsson, Alkistis Skalki-dou, Kristiina Kask, Ulla Geifalk, Margareta Nordling, Malin Helmestam, Elin Bannbers, Charlotte Hellgren and all others Anneli Stavreus Evers – for your support and scientific advices all the late evenings when we were the only ones left at research-lab All members in the Midwifery Research network - Tanja Tydén, Margareta Larsson, Gunilla Aneblom, Christine Rubertsson, Elisabeth Mattson, Kris-tina Stenson, Maria Ekstrand and all others All memebers in the PhD network - Gunn Engvall, Berit Höglund, Tiina Syvänen, Eva-Lotta Funkquist, Ylva and Christina Barbro Westerberg - for your helpfulness and patience when IT comes to IT! Lena Zetterberg - for our fruitful lunch-discussions during our PhD studies - I hope we will continue! Jane Wigertz and Sue Pajuluoma - for your skilful English revision All staff and former colleagues at the Centre of Reproduction - for doing an invaluable important work and for your support during the time of the study All staff at the Carl von Linné kliniken- for sharing interest in my studies All Midwifery colleagues and all other staff at the Department of Obstetrics and Gynaecology in Uppsala - for being supportive My whole Family - my wonderful parents, sisters and brother with families, for putting up with me and always being supportive and encouraging
Anna, Jessica and Amanda - my three lovely daughters for giving me the meaning of life! You are fantastic – you have a lot of supper-time on de-posit!

58
References
1. World Health Organization. Reproductive health. In; 2008. 2. Cullberg J. Kris och utveckling. Stockholm: Natur och Kultur; 2006. 3. Domar AD, Broome A, Zuttermeister PC, Seibel M, Friedman R. The preva-
lence and predictability of depression in infertile women. Fertil Steril. 1992;58(6):1158-63.
4. Stanton A, Dunkel-Schetter C LM. Psychological adjustment to infertility. In: Stanton A, Dunkel-Schetter C LM, editors. Infertility - Perspectives from stress and coping research; 1991.
5. Wright J, Allard M, Lecours A, Sabourin S. Psychosocial distress and infertil-ity: a review of controlled research. Int J Fertil. 1989;34(2):126-42.
6. Wirtberg I. His and her childlessness. Stockholm: Karolinska institutet; 1992. 7. Cwikel J, Gidron Y, Sheiner E. Psychological interactions with infertility
among women. Eur J Obstet Gynecol Reprod Biol. 2004;117(2):126-31. 8. National Board of Health and Welfare. Official Statistics of Sweden. 2006. 9. Templeton A, Morris JK, Parslow W. Factors that affect outcome of in-vitro
fertilisation treatment. Lancet. 1996;348(9039):1402-6. 10. Thurin A, Hardarson T, Hausken J, Jablonowska B, Lundin K, Pinborg A, et
al. Predictors of ongoing implantation in IVF in a good prognosis group of pa-tients. Hum Reprod. 2005;20(7):1876-80.
11. Bewley S, Davies M, Braude P. Which career first? BMJ. 2005;331(7517):588-9.
12. ESHRE. Good Clinical Treatment in Assisted Reproduction - An ESHRE position paper. In: 2008.
13. Lintsen AM, Pasker-de Jong PC, de Boer EJ, Burger CW, Jansen CA, Braat DD, et al. Effects of subfertility cause, smoking and body weight on the suc-cess rate of IVF. Hum Reprod. 2005;20(7):1867-75.
14. Klonoff-Cohen H. Female and male lifestyle habits and IVF: what is known and unknown Hum Reprod Update 2005;11(2):180-204.
15. Homan GF, Davies M, Norman R. The impact of lifestyle factors on reproduc-tive performance in the general population and those undergoing infertility treatment: a review. Hum Reprod Update. 2007;13(3):209-23.
16. Steptoe PC, Edwards RG. Birth after the reimplantation of a human embryo. Lancet. 1978;2(8085):366.
17. National Board of Health and Welfare. Official Statistics of Sweden. In; 2008. 18. Olivius K, Friden B, Lundin K, Bergh C. Cumulative probability of live birth
after three in vitro fertilization/intracytoplasmic sperm injection cycles. Fertil Steril. 2002;77(3):505-10.
19. Pinborg A, Hougaard CO, Nyboe Andersen A, Molbo D, Schmidt L. Prospec-tive longitudinal cohort study on cumulative 5-year delivery and adoption rates among 1338 couples initiating infertility treatment. Hum Reprod. 2009;24(4):991-9.

59
20. Nygren K, Wennerholm U. Uppföljning av IVF verksamheten. In: Hreinson J, Hamberger L, Hardarson T, editors. Infertilitet Utredning och behandling ge-nom assisterad befruktning. Lund: Studentlitteratur; 2005.
21. Klonoff-Cohen H, Chu E, Natarajan L, Sieber W. A prospective study of stress among women undergoing in vitro fertilization or gamete intrafallopian transfer. Fertil Steril. 2001;76(4):675-87.
22. Toren P, Dor J, Mester R, Mozes T, Blumensohn R, Rehavi M, et al. Depres-sion in women treated with a gonadotropin-releasing hormone agonist. Biol Psychiatry. 1996;39(5):378-82.
23. Eyal S, Rehavi M, Weizman A, Toren P, Mester R, Dor Y. Chronic GnRH agonist administration down-regulates platelet serotonin transporter in women undergoing assisted reproductive treatment. Psychopharmacology 1996;125(2):141-145.
24. Macklon NS, Stouffer RL, Giudice LC, Fauser BCJM. The Science behind 25 Years of Ovarian Stimulation for in Vitro Fertilization Endocr Rev 2006;27(2):170-207.
25. de Klerk C, Macklon NS, Heijnen EMEW, Eijkemans MJC, Fauser BCJM, Passchier J, et al. The psychological impact of IVF failure after two or more cycles of IVF with a mild versus standard treatment strategy Hum. Reprod. 2007;22(9):2554-2558.
26. de Klerk C, Heijnen EMEW, Macklon NS, Duivenvoorden HJ, Fauser BCJM, Passchier J, et al. The psychological impact of mild ovarian stimulation com-bined with single embryo transfer compared with conventional IVF Hum. Re-prod. 2006;21(3):721-727.
27. Slade P, Emery J, Lieberman BA. A prospective, longitudinal study of emo-tions and relationships in in-vitro fertilization treatment. Hum Reprod. 1997;12(1):183-90.
28. Demyttenaere K, Bonte L, Gheldof M, Vervaeke M, Meuleman C, Vander-schuerem D, et al. Coping style and depression level influence outcome in in vitro fertilization. Fertil Steril. 1998;69(6):1026-33.
29. Hammarberg K, Astbury J, Baker H. Women's experience of IVF: a follow-up study. Hum Reprod. 2001;16(2):374-83.
30. Verhaak CM, Smeenk JM, Evers AW, van Minnen A, Kremer JA, Kraaimaat FW. Predicting emotional response to unsuccessful fertility treatment: a pro-spective study. J Behav Med 2005;28(2):181-90.
31. Sbaragli C, Morgante G, Goracci A, Hofkens T, De Leo V, Castrogiovanni P. Infertility and psychiatric morbidity. Fertil Steril. 2008;90(6):2107-11.
32. Csemiczky G, Landgren BM, Collins A. The influence of stress and state anxiety on the outcome of IVF-treatment: psychological and endocrinological assessment of Swedish women entering IVF-treatment. Acta Obstet Gynecol Scand. 2000;79(2):113-8.
33. Tica VI, Mares P, Gouzes C, Badea P, Popescu G, Tica I. The variation of serum cortisol during ovarian stimulation for in vitro fertilization. Gynecol Endocrinol. 2008;24(1):12-7.
34. Baumeister H, Maercker A, Casey P. Adjustment disorder with depressed mood: a critique of its DSM-IV and ICD-10 conceptualisations and recom-mendations for the future. Psychopathology 2009;42(3):139-47.
35. American Psychiatric Association. MINI-D IV: Pilgrim Press; 2002. 36. Kessler R. The effects of stressful life events on depression. Annu Rev Psy-
chol. 1997;48:191-214.

60
37. Cyranowski JM, Frank E, Young E, Shear MK. Adolescent onset of the gen-der difference in lifetime rates of major depression: a theoretical model. Arch Gen Psychiatry. 2000;57(1):21-7.
38. Nesse RM. Is Depression an Adaptation? Arch Gen Psychiatry 2000;57(1):14-20.
39. Menning BE. The emotional needs of infertile couples. Fertil Steril. 1980;34(4):313-9.
40. Caplan G, Mason EA, Kaplan DM. Four studies of crisis in parents of prema-tures. Community Ment Health J. 2000;36(1):25-45.
41. Caplan G. Principles of preventive psychiatry. New York: Basic Books; 1964. 42. Wirtberg I, Moller A, Hogstrom L, Tronstad SE, Lalos A. Life 20 years after
unsuccessful infertility treatment. Hum Reprod. 2007;22(2):598-604. 43. Lalos A, Lalos O, Jacobsson L, von Schoultz B. Depression, guilt and isola-
tion among infertile women and their partners. J of Psychosomatic Obstetrics and Gynaecology 1986;5:197-206.
44. Mahlstedt PP. The psychological component of infertility. Fertil Steril. 1985;43(3):335-46.
45. Lindemann E. Symptomatology and management of acute grief. 1944. Am J Psychiatry. 1994;151(6 Suppl):155-60.
46. ACOG. Depression in women. ACOG technical bulletin number 182--July 1993. Int J Gynaecol Obstet. 1993;43(2):203-11.
47. Williams K, Zappert L. Psychopathology and psychopharmacology in the infertile patient. NY, USA: Cambridge University Press,; 2006.
48. Maercker A. When grief becomes a disorder. Eur Arch Psychiatry Clin Neuro-sci. 2007;257(8):435-6.
49. American Psychiatric Association. Diagnostic and statistical manual of mental disorders; DSM-IV. Washington; 1994.
50. Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8-19.
51. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Life-time Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication Arch Gen Psychiatry 2005;62(6):593-602.
52. Kringlen E, Torgersen S, Cramer V. A Norwegian psychiatric epidemiological study. Am J Psychiatry. 2001;158(7):1091-8.
53. Kringlen E, Torgersen S, Cramer V. Mental illness in a rural area: a Norwe-gian psychiatric epidemiological study. Soc Psychiatry Psychiatr Epidemiol. 2006;41(9):713-9.
54. Breslau N, Schultz L, Peterson E. Sex differences in depression: a role for preexisting anxiety. Psychiatry Res. 1995;58(1):1-12.
55. Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Co-morbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617-27.
56. Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341(18):1329-35.
57. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349(9064):1498-504.

61
58. Wells KB, Stewart A, Hays RD, Burnam MA, Rogers W, Daniels M, et al. The functioning and well-being of depressed patients. Results from the Medi-cal Outcomes Study. JAMA. 1989;262(7):914-9.
59. Paykel ES. Basic concepts of depression. Dialogues Clin Neurosci 2008;10(3):279-89.
60. Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74(1):5-13.
61. Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major de-pressive disorder: results from the National Epidemiologic Survey on Alcohol-ism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097-106.
62. Tuccori M, Testi A, Antonioli L, Fornai M, Montagnani S, Ghisu N, et al. Safety concerns associated with the use of serotonin reuptake inhibitors and other serotonergic/noradrenergic antidepressants during pregnancy: A review. Clinical Therapeutics Mental health disorders 2009;31(Part 1):1426-1453.
63. Chambers CD, Hernandez-Diaz S, Van Marter LJ, Werler MM, Louik C, Jones KL, et al. Selective Serotonin-Reuptake Inhibitors and Risk of Persistent Pulmonary Hypertension of the Newborn N Engl J Med 2006;354(6):579-587.
64. Medical Products Agency. Gravida bor ej avbryta behandling mot depression. In; 2006.
65. Feldman G. Cognitive and behavioral therapies for depression: overview, new directions, and practical recommendations for dissemination. Psychiatr Clin North Am. 2007;30(1):39-50.
66. Domar AD, Friedman R, Zuttermeister PC. Distress and conception in infertile women: a complementary approach. J Am Med Womens Assoc. 1999;54(4):196-8.
67. Facchinetti F, Tarabusi M, Volpe A. Cognitive-behavioral treatment decreases cardiovascular and neuroendocrine reaction to stress in women waiting for as-sisted reproduction. Psychoneuroendocrinology. 2004;29(2):162-73.
68. Chen TH, Chang SP, Tsai CF, Juang KD. Prevalence of depressive and anxi-ety disorders in an assisted reproductive technique clinic. Hum Reprod. 2004;19(10):2313-8.
69. Guerra D, Llobera A, Veiga A, Barri PN. Psychiatric morbidity in couples attending a fertility service. Hum Reprod. 1998;13(6):1733-6.
70. Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV, 3rd, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272(22):1749-56.
71. Lok IH, Lee DT, Cheung LP, Chung WS, Lo WK, Haines CJ. Psychiatric morbidity amongst infertile Chinese women undergoing treatment with as-sisted reproductive technology and the impact of treatment failure. Gynecol Obstet Invest. 2002;53(4):195-9.
72. Anderson K, Sharpe M, Rattray A, Irvine D. Distress and concerns in couples referred to a specialist infertility clinic. J Psychosom Res. 2003;54(4):353-5.
73. Williams KE, Marsh WK, Rasgon NL. Mood disorders and fertility in women: a critical review of the literature and implications for future research. Hum Reprod Update. 2007;13(6):607-16.
74. Verhaak CM, Smeenk JM, Evers AW, Kremer JA, Kraaimaat FW, Braat DD. Women's emotional adjustment to IVF: a systematic review of 25 years of re-search. Hum Reprod Update. 2006;13(1):27-36.
75. Newton CR, Hearn MT, Yuzpe AA. Psychological assessment and follow-up after in vitro fertilization: assessing the impact of failure. Fertil Steril. 1990;54(5):879-86.

62
76. Kessler RC, Magee WJ. Childhood adversities and adult depression: basic patterns of association in a US national survey. Psychol Med. 1993;23(3):679-90.
77. Kendler KS, Thornton LM, Gardner CO. Stressful life events and previous episodes in the etiology of major depression in women: an evaluation of the "kindling" hypothesis. Am J Psychiatry. 2000;157(8):1243-51.
78. Baumeister H, Harter M. Prevalence of mental disorders based on general population surveys. Soc Psychiatry Psychiatr Epidemiol. 2007;42(7):537-46.
79. Andersson L, Sundstrom-Poromaa I, Wulff M, Astrom M, Bixo M. Implica-tions of antenatal depression and anxiety for obstetric outcome. Obstet Gyne-col. 2004;104(3):467-76.
80. Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63(7):824-30.
81. Barry D, Pietrzak RH, Petry NM. Gender differences in associations between body mass index and DSM-IV mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Ann Epi-demiol. 2008;18(6):458-66.
82. Atlantis E, Baker M. Obesity effects on depression: systematic review of epi-demiological studies. Int J Obes (Lond). 2008;32(6):881-91.
83. Connolly KJ, Edelmann RJ, Cooke ID, Robson J. The impact of infertility on psychological functioning. J Psychosom Res. 1992;36(5):459-68.
84. Lukse MP, Vacc NA. Grief, depression, and coping in women undergoing infertility treatment. Obstet Gynecol. 1999;93(2):245-51.
85. Caspi A, Roberts BW, Shiner RL. Personality development: stability and change. Annu Rev Psychol. 2005;56:453-84.
86. Costa PT, Jr., McCrae RR. Personality in adulthood: a six-year longitudinal study of self-reports and spouse ratings on the NEO Personality Inventory. J Pers Soc Psychol. 1988;54(5):853-63.
87. Gustavsson JP, Weinryb RM, Göransson S, Pedersend NL, Åsberg M. Stabil-ity and predictive ability of personality traits across 9 years. Person. indiv. Diff. 1997;22(6):783-791.
88. Santor DA, Bagby RM, Joffe RT. Evaluating stability and change in personal-ity and depression. J Pers Soc Psychol. 1997;73(6):1354-62.
89. Neeleman J, Sytema S, Wadsworth M. Propensity to psychiatric and somatic ill-health: evidence from a birth cohort. Psychol Med. 2002;32(5):793-803.
90. Hirschfeld RM, Klerman GL, Clayton PJ, Keller MB. Personality and depres-sion. Empirical findings. Arch Gen Psychiatry. 1983;40(9):993-8.
91. Kendler KS, Kessler RC, Neale MC, Heath AC, Eaves LJ. The prediction of major depression in women: toward an integrated etiologic model. Am J Psy-chiatry. 1993;150(8):1139-48.
92. Shea MT, Leon AC, Mueller TI, Solomon DA, Warshaw MG, Keller MB. Does major depression result in lasting personality change? Am J Psychiatry. 1996;153(11):1404-10.
93. Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. J Abnorm Psychol. 1994;103(1):103-16.
94. Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. A longitudinal twin study of personality and major depression in women. Arch Gen Psychiatry. 1993;50(11):853-62.
95. Kendler KS, Neale M, Kessler R, Heath A, Eaves L. A twin study of recent life events and difficulties. Arch Gen Psychiatry. 1993;50(10):789-96.

63
96. Litt MD, Tennen H, Affleck G, Klock S. Coping and cognitive factors in ad-aptation to in vitro fertilization failure. J Behav Med. 1992;15(2):171-87.
97. Imeson M, McMurray A. Couples' experiences of infertility: a phenomenol-ogical study. J Adv Nurs. 1996;24(5):1014-22.
98. Bryson CA, Sykes DH, Traub AI. In vitro fertilization: a long-term follow-up after treatment failure. Hum Fertil (Camb). 2000;3(3):214-220.
99. Filetto JN, Makuch MY. Long-term follow-up of women and men after un-successful IVF. Reprod Biomed Online. 2005;11(4):458-63.
100. Verhaak CM, Smeenk JM, Nahuis MJ, Kremer JA, Braat DD. Long-term psychological adjustment to IVF/ICSI treatment in women. Hum Reprod. 2007;22(1):305-8.
101. Johansson M, Berg M. Women's experiences of childlessness 2 years after the end of in vitro fertilization treatment. Scand J Caring Sci. 2005;19(1):58-63.
102. Bergart AM. The experience of women in unsuccessful infertility treatment: what do patients need when medical intervention fails? Soc Work Health Care. 2000;30(4):45-69.
103. McCarthy MP. Women's lived experience of infertility after unsuccessful medical intervention. J Midwifery Womens Health. 2008;53(4):319-24.
104. Schmidt L. Infertile couples' assessment of infertility treatment. Acta Obstet Gynecol Scand. 1998;77(6):649-53.
105. Daniluk JC. Reconstructing Their Lifes; A longitudinal, Qualitative Analysis of the Transition to Biological Childlessness for Infertile Couples. J Counsel Dev 2001;79:439-449.
106. Boden J. When IVF treatment fails. Hum Fertil (Camb). 2007;10(2):93-8. 107. Kobak KA, Taylor LH, Dottl SL, Greist JH, Jefferson JW, Burroughs D, et al.
A computer-administered telephone interview to identify mental disorders. JAMA. 1997;278(11):905-10.
108. Beekman AT, Deeg DJ, Braam AW, Smit JH, Van Tilburg W. Consequences of major and minor depression in later life: a study of disability, well-being and service utilization. Psychol Med. 1997;27(6):1397-409.
109. Schalling D, Asberg M, Edman G, Oreland L. Markers for vulnerability to psychopathology: temperament traits associated with platelet MAO activity. Acta Psychiatr Scand. 1987;76(2):172-82.
110. Gustavsson JP, Bergman H, Edman G, Ekselius L, von Knorring L, Linder J. Swedish universities Scales of Personality (SSP): construction, internal consis-tency and normative data. Acta Psychiatr Scand. 2000;102(3):217-25.
111. Willebrand M, Kildal M, Andersson G, Ekselius L. Long-term assessment of personality after burn trauma in adults. J Nerv Ment Dis. 2002;190(1):53-6.
112. Bagley SC, White H, Golomb BA. Logistic regression in the medical litera-ture: standards for use and reporting, with particular attention to one medical domain. J Clin Epidemiol. 2001;54(10):979-85.
113. Hosmer D, Lemeshow S. Applied Logistic Regression: Wiley Inc.; 2000. 114. Pallant J. SPSS Survival Manual. 3rd ed: Open University Press; 2007. 115. Graneheim UH, Lundman B. Qualitative content analysis in nursing research:
concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105-12.
116. Kvale S, Berinkmann S. Den kvalitativa forskningsintervjun. Lund: Studentlit-teratur; 2009.
117. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737-44.

64
118. Wells KB, Burnam MA, Leake B, Robins LN. Agreement between face-to-face and telephone-administered versions of the depression section of the NIMH Diagnostic Interview Schedule. J Psychiatr Res. 1988;22(3):207-20.
119. Evans M, Kessler D, Lewis G, Peters TJ, Sharp D. Assessing mental health in primary care research using standardized scales: can it be carried out over the telephone? Psychol Med. 2004;34(1):157-62.
120. Kendler KS, Gatz M, Gardner CO, Pedersen NL. Personality and major de-pression: a Swedish longitudinal, population-based twin study. Arch Gen Psy-chiatry. 2006;63(10):1113-20.
121. Enns MW, Cox BJ. Personality dimensions and depression: review and com-mentary. Can J Psychiatry. 1997;42(3):274-84.
122. Parker DA, Parker ES, Harford TC, Farmer GC. Alcohol use and depression symptoms among employed men and women. Am J Public Health. 1987;77(6):704-7.
123. Ansseau M, Dierick M, Buntinkx F, Cnockaert P, De Smedt J, Van Den Haute M, et al. High prevalence of mental disorders in primary care. J Affect Disord. 2004;78(1):49-55.
124. Beutel M, Kupfer J, Kirchmeyer P, Kehde S, Kohn FM, Schroeder-Printzen I, et al. Treatment-related stresses and depression in couples undergoing assisted reproductive treatment by IVF or ICSI. Andrologia. 1999;31(1):27-35.
125. Sundstrom IM, Bixo M, Bjorn I, Astrom M. Prevalence of psychiatric disor-ders in gynecologic outpatients. Am J Obstet Gynecol. 2001;184(2):8-13.
126. Andersson L, Sundstrom-Poromaa I, Bixo M, Wulff M, Bondestam K, Åstrom M. Point prevalence of psychiatric disorders during the second trimester of pregnancy: a population-based study. Am J Obstet Gynecol. 2003;189(1):148-54.
127. Bergsjø P. Qualitative and quantitative research, Is there a gap, or only verbal disagreement? Acta Obstet Gynecol Scand. 1999 Aug;78(7):559-62 1999;78(7):559-62.
128. Malterud K. The art and science of clinical knowledge: evidence beyond measures and numbers. Lancet. 2001;358(9279):397-400.
129. Peddie VL, van Teijlingen E, Bhattacharya S. A qualitative study of women's decision-making at the end of IVF treatment. Hum Reprod. 2005;20(7):1944-51.
130. Peddie V, van Teijlingen E. Qualitative research in fertility and reproduction: Does it have any value? Human Fertility 2005;8(4):263-267.
131. Malterud K. Kvalitativa metoder i medicinsk forskning. Lund: Studentlittera-tur; 1998.
132. Malterud K. Shared understanding of the qualitative research process. Guide-lines for the medical researcher. Fam Pract. 1993;10(2):201-6.
133. Boivin J, Scanlan LC, Walker S. Why are infertile patients not using psycho-social counselling? Hum Reprod. 1999;14(5):1384-91.
134. Anderheim L, Holter H, Bergh C, Moller A. Extended encounters with mid-wives at the first IVF cycle: a controlled trial. Reproductive BioMedicine Online;14:279-287.
135. Hammerli K, Znoj H, Barth J. The efficacy of psychological interventions for infertile patients: a meta-analysis examining mental health and pregnancy rate Hum Reprod Update 2009;15(3):279-295.
136. Verhaak CM, Smeenk JM, Eugster A, van Minnen A, Kremer JA, Kraaimaat FW. Stress and marital satisfaction among women before and after their first cycle of in vitro fertilization and intracytoplasmic sperm injection. Fertil Steril. 2001;76(3):525-31.

65
137. Yonkers KA, Wisner KL, Stewart DE, Oberlander TF, Dell DL, Stotland N, et al. The management of depression during pregnancy: a report from the Ameri-can Psychiatric Association and the American College of Obstetricians and Gynecologists. General Hospital Psychiatry 2009;31(5):403-413.
138. Einarson A, Choi J, Einarson T, Koren G. Adverse effects of antidepressant use in pregnancy: an evaluation of fetal growth and preterm birth. Depress Anxiety. 2009;[Epub ahead of print].
139. Hollinrake E, Abreu A, Maifeld M, Van Voorhis BJ, Dokras A. Increased risk of depressive disorders in women with polycystic ovary syndrome. Fertil Steril. 2007;87(6):1369-76.
140. Galletly C, Clark A, Tomlinson L, Blaney F. Improved pregnancy rates for obese, infertile women following a group treatment program. An open pilot study. Gen Hosp Psychiatry. 1996;18(3):192-5.
141. Maheshwari A, Stofberg L, Bhattacharya S. Effect of overweight and obesity on assisted reproductive technology--a systematic review. Hum Reprod Up-date. 2007;13(5):433-44.
142. Lalos A. Breaking bad news concerning fertility. Hum Reprod. 1999;14(3):581-5.
143. Sundby J, Schmidt L, Heldaas K, Bugge S, Tanbo T. Consequences of IVF among women: 10 years post-treatment. J Psychosom Obstet Gynaecol. 2007;28(2):115-20.
144. Lancastle D, Boivin J. Dispositional optimism, trait anxiety, and coping: unique or shared effects on biological response to fertility treatment? Health Psychol. 2005;24(2):171-8.
145. Thiering P, Beaurepaire J, Jones M, Saunders D, Tennant C. Mood state as a predictor of treatment outcome after in vitro fertilization/embryo transfer technology (IVF/ET). J Psychosom Res. 1993;37(5):481-91.
146. Facchinetti F, Matteo ML, Artini GP, Volpe A, Genazzani AR. An increased vulnerability to stress is associated with a poor outcome of in vitro fertiliza-tion-embryo transfer treatment. Fertil Steril. 1997;67(2):309-14.
147. Smeenk JM, Verhaak CM, Eugster A, van Minnen A, Zielhuis GA, Braat DD. The effect of anxiety and depression on the outcome of in-vitro fertilization. Hum Reprod. 2001;16(7):1420-3.
148. Milad MP, Klock SC, Moses S, Chatterton R. Stress and anxiety do not result in pregnancy wastage. Hum Reprod. 1998;13(8):2296-300.
149. Ardenti R, Campari C, Agazzi L, La Sala GB. Anxiety and perceptive func-tioning of infertile women during in-vitro fertilization: exploratory survey of an Italian sample. Hum Reprod. 1999;14(12):3126-32.
150. Lintsen AM, Verhaak CM, Eijkemans MJ, Smeenk JM, Braat DD. Anxiety and depression have no influence on the cancellation and pregnancy rates of a first IVF or ICSI treatment. Hum Reprod. 2009.
151. de Klerk C, Hunfeld JA, Heijnen EM, Eijkemans MJ, Fauser BC, Passchier J, et al. Low negative affect prior to treatment is associated with a decreased chance of live birth from a first IVF cycle. Hum Reprod. 2008;23(1):112-6.
152. Lechner L, Bolman C, van Dalen A. Definite involuntary childlessness: asso-ciations between coping, social support and psychological distress. Hum Re-prod. 2007;22(1):288-94.
153. Olivius C, Friden B, Borg G, Bergh C. Why do couples discontinue in vitro fertilization treatment? A cohort study. Fertil Steril. 2004;81(2):258-61.
154. Verberg MF, Eijkemans MJ, Heijnen EM, Broekmans FJ, de Klerk C, Fauser BC, et al. Why do couples drop-out from IVF treatment? A prospective cohort study. Hum Reprod. 2008;23(9):2050-5.

66
155. Lok IH, Neugebauer R. Psychological morbidity following miscarriage. Best Pract Res Clin Obstet Gynaecol. 2007;21(2):229-47.
156. Levitt C. Vulnerability in Women with Infertility. In: de Chesney M, editor. Caring for the Vulnerable: Jones and Bartlett; 2005.
157. Mourad SM, Hermens RPMG, Cox-Witbraad T, Grol RPTM, Nelen WLDM, Kremer JAM. Information provision in fertility care: a call for improvement Hum. Reprod. 2009;24(6):1420-1426.

1. Magont
2. Ryggont
3. Smärta i armar,ben, leder (höfter,knän etc)
4. Smärtor ellerproblem vidmenstruation
5. Smärtor ellerproblem vidsamlag
6. Huvudvärk
7. Smärtor i brösteteller tryck överbröstet
8. Yrsel
9. Svimningar
10. Hjärtklappning
11. Andnöd
12. Förstoppning,lös avföring ellerdiarre
13. Illamående,gasbildning ellermatsmältnings-problem
14. Trötthet ellerbristande energi
15. Sömnproblem
16. Tappat kontrollenöver ätandet
17. Minskad lust attgöra saker somDu vanligentycker om
18. Att Du har käntDig illa till mods,deprimerad ellerkänt att framtidenser hopplös ut
19. Nervositet,ångest eller oro
20. Ängslan övermånga olika saker
21. Har Du haft enplötslig känsla avångest eller panik?
22. Har Du återkommandeidéer, fantasier ellerimpulser som verkardumma, konstiga,frånstötande ellerhemska?
23. Finns det saker som Dugör om och om igen,eller tankar Du måstetänka upprepade gångerför att känna Dig lugn?
24. Är Du rädd för att bligenerad ellerförödmjukad i socialasituationer ochundviker Du sådanasituationer?
Under senaste månaden
Har Du under den senaste månaden ofta haft......
JA NEJ JA NEJ JA NEJ
FRÅGEFORMULÄR
Namn:
Telefon hemma:
VÄGLEDNING: Det är viktigt att Du fyller i JA eller NEJ på samtliga 25 frågor.
Födelsedata (år, mån, dag):
Mobiltelefon:
I det stora hela skulle Dubeskriva Din hälsa som:
PerfektUtmärktGodMindre godDålig

APPENDIX
1. DSM-IV criteria
Major depressive episode
A. Five (or more) of the following symptoms have been present during the same two-week
period and represent a change from previous functioning; at least one of the symptoms is either
(1) depressed mood or
(2) loss of interest or pleasure.
Note: Do not include symptoms that are clearly due to a general medical condition, or mood-
incongruent delusions or hallucinations.
(1) Depressed mood most of the day, nearly every day, as indicated by either subjective
report (for example, feels sad or empty) or observations made by others (for example,
appears tearful). Note: In children and adolescents, can be irritable mood.
(2) Marked diminished interest or pleasure in all, or almost all, activities most of the day,
nearly every day (as indicated by either subjective account or observation made by
others).
(3) Significant weight loss when not dieting or weight gain (for example, change of more
than 5% of body weight in a month), or decrease or increase in appetite nearly every day.
Note: In children, consider failure to make expected weight gains.
(4) Insomnia or hypersomnia nearly every day.
(5) Psychomotor agitation or retardation nearly every day (observable by others, not merely
subjective feelings of restlessness or being slowed down).
(6) Fatigue or loss of energy nearly every day.
(7) Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional)
nearly every day (not merely self-reproach or guilt about being sick).
(8) Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by
subjective account or as observed by others).
(9) Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a
specific plan, or a suicide attempt or a specific plan for committing suicide.
B. The symptoms do not meet criteria for a mixed episode.

C. The symptoms cause clinically significant distress or impairment in social, occupational, or
other important areas of functioning.
D. The symptoms are not due to the direct physiological effects of a substance (for example, a
drug of abuse, a medication) or a general medical condition (for example, hypothyroidism).
E. The symptoms are not better accounted for by bereavement, that means, after the loss of a
loved one, the symptoms persist for longer than two months or are characterized by marked
functional impairment, morbid preoccupation with worthlessness, suicidal ideation, psychotic
symptoms, or psychomotor retardation.
Dysthymic disorder
A. Depressed mood for most of the day, for more days than not, as indicated either by subjective
account or observation by others, for at least two years. Note: In children and adolescents, mood
can be irritable and duration must be at least one year.
B. Presence, while depressed, of two (or more) of the following:
(1) poor appetite or overeating
(2) insomnia or hypersomnia
(3) low energy or fatigue
(4) low self-esteem
(5) poor concentration or difficulty making decisions
(6) feelings of hopelessness
C. During the two-year period (one year for children or adolescents) of the disturbance, the
person has never been without the symptoms in criteria A and B for more than two months at a
time.
D. No major depressive episode has been present during the first two years of the disturbance
(one year for children and adolescents); i.e., the disturbance is not better accounted for by
chronic major depressive disorders, or major depressive disorder, in partial remission. Note:
There may have been a previous major depressive episode provided there was a full remission
(no significant signs or symptoms for two months) before development of the dysthymic
disorder. In addition, after the initial two years (one year in children or adolescents) of dysthymic
disorder, there may be superimposed episodes of major depressive disorder, in which case both
diagnoses may be given when the criteria are met for a major depressive episode.
E. There has never been a manic episode, a mixed episode, or a hypomanic episode, and criteria
have never been met for cyclothymic disorders.

F. The disturbance does not occur exclusively during the course of a chronic psychotic disorder,
such as schizophrenia or delusional disorder.
G. The symptoms are not due to the direct physiological effects of a substance (for example, a
drug of abuse, a medication) or a general medical condition (for example., hypothyroidism).
H. The symptoms cause clinically significant distress or impairment in social, occupational, or
other important areas of functioning.
Generalized anxiety disorder
A. Excessive anxiety and worry (apprehensive expectation), occurring more days than not for at
least six months, about a number of events or activities (such as work or school performance).
B. The person finds it difficult to control the worry.
C. The anxiety and worry are associated with three (or more) of the following six symptoms (with
at least some symptoms present for more days than not for the past six months. Note: Only one
item is required in children.
(1) restlessness or feeling keyed up or on the edge
(2) being easily fatigued
(3) difficult concentrating or mind going blank
(4) irritability
(5) muscle tension
(6) sleep disturbance (difficult falling or staying asleep, or restless unsatisfying sleep)
D. The focus of the anxiety and worry is not confined to features of an axis I disorder, for
example, the anxiety or worry is not about having a panic attack (as in panic disorder), being
embarrassed in public (as in social phobia), being contaminated (as in obsessive-compulsive
disorder), being away from home or close relatives (as in separation anxiety disorder), gaining
weight (as in anorexia nervosa), having multiple physical complaints (as in somatization disorder),
or having a serious illness (as in hypochondriasis), and the anxiety and worry do not occur
exclusively during posttraumatic stress disorder.
E. The anxiety, worry or physical symptoms cause clinically significant distress or impairment in
social, occupational, or other important areas of functioning.
F. The disturbance is not due to the direct physiological effects of a substance (for example, a
drug of abuse, a medication) or a general medical condition (for example, hyperthyroidism) and
do not occur exclusively during a mood disorder, a psychotic disorder, or a pervasive
developmental disorder.

Panic disorder without agoraphobia
A. Both (1) and (2):
(1) recurrent unexpected panic attacks
(2) at least one of the attacks has been followed by one month (or more) of one
(or more) of the following:
(a) persistent concern about having additional attacks
(b) worry about the implications of the attack or its consequences
(for example., losing control, having a heart attack, "going crazy")
(c) a significant change in behavior related to the attacks
B. Absence of agoraphobia.
C. The panic attacks are not due to the direct physiological effects of a substance (for example, a
drug of abuse, a medication) or a general medical condition (e.g., hyperthyroidism).
D. The panic attacks are not better accounted for by another mental disorder, such as social
phobia (for example, occurring on exposure to feared social situations), specific phobia (for
example, on exposure to a specific phobic situation), obsessive-compulsive disorder (for example,
on exposure to dirt in someone with an obsession about contamination), posttraumatic stress
disorder (for example, in response to stimuli associated with a severe stressor), or separation
anxiety disorder (for example, in response to being away from home or close relatives).
Obsessive-compulsive disorder
A. Either obsessions or compulsions:
Obsessions as defined by (1), (2), (3), and (4):
(1) recurrent and persistent thoughts, impulses, or images that are experienced, at
some time during the disturbance, as intrusive and inappropriate and that cause
marked anxiety or distress
(2) the thoughts, impulses, or images are not simply excessive worries about real-
life problems
(3) the person attempts to ignore or suppress such thoughts, impulses, or images,
or to neutralize them with some other thought or action
(4) the person recognizes that the obsessional thoughts, impulses, or images are a
product of his or her own mind (not imposed from without as in thought
insertion)

Compulsions as defined by (1) and (2):
(1) repetitive behaviors (for example, hand washing, ordering, checking) or mental
acts (for example, praying, counting, repeating words silently) that the person
feels driven to perform in response to an obsession, or according to rules that
must be applied rigidly
(2) the behaviors or mental acts are aimed at preventing or reducing distress or
preventing some dreaded event or situation; however, these behaviors or mental
acts either are not connected in a realistic way with what they are designed to
neutralize or prevent or are clearly excessive
B. At some point during the course of the disorder, the person has recognized that the
obsessions or compulsions are excessive or unreasonable. Note: This does not apply to children.
C. The obsessions or compulsions cause marked distress, are time consuming (take more than
one hour a day), or significantly interfere with the person’s normal routine, occupational (or
academic) functioning, or usual social activities or relationships.
D. If another Axis I disorder is present, the content of the obsessions or compulsions is not
restricted to it (for example, preoccupation with food in the presence of an eating disorder; hair
pulling in the presence of trichotillomania; concern with appearance in the presence of body
dysmorphic disorder; preoccupation with drugs in the presence of a substance use disorder;
preoccupation with having a serious illness in the presence of hypochondriasis; preoccupation
with sexual urges or fantasies in the presence of a paraphilia; or guilty ruminations in the presence
of major depressive disorder).
E. The disturbance is not due to the direct physiological effects of a substance (for example, a
drug of abuse, a medication) or a general medical condition.
Specify if:
With poor insight: if, for most of the time during the current episode the person does not
recognize that the obsessions and compulsions are excessive or unreasonable.
Social phobia
A. A marked and persistent fear of one or more social or performance situations in which the
person is exposed to unfamiliar people or to possible scrutiny by others. The individual fears that
he or she will act in a way (or show anxiety symptoms) that will be humiliating or embarrassing.
Note: In children, there must be evidence of the capacity for age-appropriate social relationships
with familiar people and the anxiety must occur in peer settings, not just in interactions with
adults.

B. Exposure to the feared social situation almost invariably provokes anxiety, which may take the
form of a situationally bound or situationally predisposed panic attack. Note: In children, the
anxiety may be expressed by crying, tantrums, freezing, or shrinking from social situations with
unfamiliar people.
C. The person recognizes that the fear is excessive or unreasonable. Note: In children, this
feature may be absent.
D. The feared social or performance situations are avoided or else are endured with intense
anxiety or distress.
E. The avoidance, anxious anticipation, or distress in the feared social or performance situation(s)
interferes significantly with the person's normal routine, occupational (academic) functioning, or
social activities or relationships, or there is marked distress about having the phobia.
F. In individuals under age 18 years, the duration is at least 6 months.
G. The fear or avoidance is not due to the direct physiological effects of a substance (for
example, a drug of abuse, a medication) or a general medical condition and is not better
accounted for by another mental disorder (for example, panic disorder with or without
agoraphobia, separation anxiety disorder, body dysmorphic disorder, a pervasive developmental
disorder, or schizoid personality disorder).
H. If a general medical condition or another mental disorder is present, the fear in criterion A is
unrelated to it; for example, the fear is not of stuttering, trembling in Parkinson’s disease, or
exhibiting abnormal eating behavior in anorexia nervosa or bulimia nervosa.
Specify if: Generalized: if the fears include most social situations (also consider the additional
diagnosis of avoidant personality disorder).

"3�����4 ��������5��� ������������� �������������� ������������������� ������� ����������������������������
��������6 � �������6 ���3��������� �3�
"���3��������� �������������6 ���3��������� �3� ���55������4 ����������������������������������� �����5�5 ��7�"�� 83�5 ������6 �3��5� � ���� ��������� �9 5�������:���%8 ��6� � ��36������ ���86� ��6 ������������� ���������� ��� ������������6����6��6 �� � �������;��5� 6 ��4 %����� ������55������� ��������������6 ���3�������� �3� 7�<��������=��������+,,)���6 �� � ��8���5����6 ���� ���6 ���� �>;��5� 6 ��4 �%����� ������55������ ��������������6 ���3��������� �3� ?7@
����������5���3�����7��7� ��������� �����4�*',��(�
������������������� ���������� �����

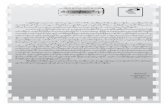



![Untitled-2 []...˘ˇ ˆ ˙ ˇ ˙ ˝ ˛ ˚ˆ ˇ ˛ ˆ ˜ ˆ ˜ ˛ ˆˆ˙ !" # ˙ ˇ ˆ $ ˜ˆ ˆˆ $ ˛ ˙ ˛ ˛ ˆ ˆ ˜ ˆ ˆ $ ˝ ˛ ˚ˆ ˇ ˛ ˙ ˇ ˆ ˇˇ ˆˆ ...](https://static.fdocuments.us/doc/165x107/5e66db259e270c079278a430/untitled-2-oe-oe-.jpg)